After years of treating ulcerative colitis symptoms without finding relief, Carolyn turned to Tiny Health. Her Gut Test revealed specific bacterial imbalances that research links to colitis and IBS. With personalized dietary changes and targeted probiotics, she eliminated her colitis symptoms.
Case Study: How Gut Test Data Helped Carolyn Overcome Colitis

Summary
As a Lutheran pastor, wife, and mother of two, Carolyn's life keeps her on the move. But showing up fully for all that she loves wasn't always simple.
Carolyn’s health challenges started early—Hashimoto’s thyroiditis in middle school, ulcerative colitis in her 20s, followed by fatigue and weight gain after becoming a parent. Later, Carolyn and her husband, also a Lutheran pastor, faced a rare disease diagnosis with their newborn son. As a healthcare professional, these life experiences deepened Carolyn’s curiosity about medical breakthroughs, preventive care, and the gut microbiome.
We caught up with Carolyn recently, and she opened up about her gut health progress, frustrations with healthcare, and how she was able to taper off medications she never thought possible. Her story is a powerful reminder that advocating for yourself and understanding the root causes of your symptoms can lead to real change.
Treating symptoms, missing answers
Living with ulcerative colitis meant Carolyn dealt with uncomfortable, sometimes alarming symptoms daily. "I used to have blood and mucus in my stools," she shares. Ulcerative colitis is a chronic condition that causes inflammation and sores in the large intestine, leading to symptoms like diarrhea, abdominal pain, and blood in the stool. It’s linked to an overactive immune response and imbalances in gut bacteria.
Carolyn was on anti-inflammatory medications to manage her colitis and thyroid medication for Hashimoto's. Hashimoto's thyroiditis is an autoimmune condition in which the immune system attacks the thyroid, often leading to low thyroid hormone levels and symptoms such as fatigue, weight gain, and changes in metabolism and energy.
But it wasn’t just the symptoms that troubled her.
"I was frustrated with my experience seeing gastroenterologists because their answer was always 'here, take this medication which calms the inflammation' rather than 'maybe we should dive into why there is inflammation in your colon in the first place."
That pattern — never investigating the underlying cause, treating each condition in isolation rather than holistically — was draining.
Carolyn couldn't shake the feeling that there had to be a better way forward. That's when she connected with a nurse practitioner at the Penny George Institute for Health and Healing. Her functional medicine practitioner suggested a Tiny Health Gut Health Test, and it turned out to be the breakthrough she'd been searching for.
What Carolyn’s gut health test revealed
When her results came back, Carolyn’s practitioner walked her through her report and what was happening in her gut.
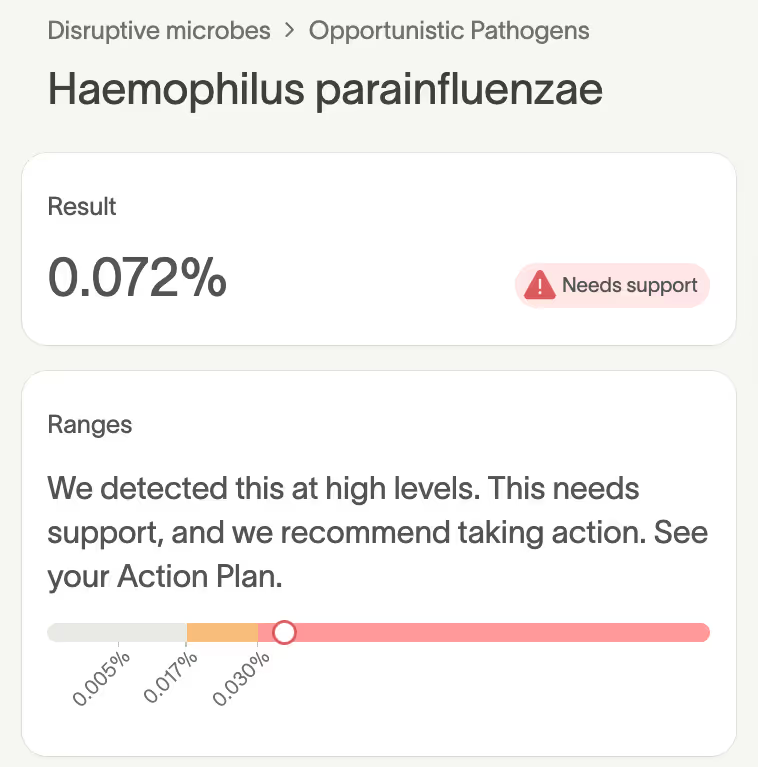
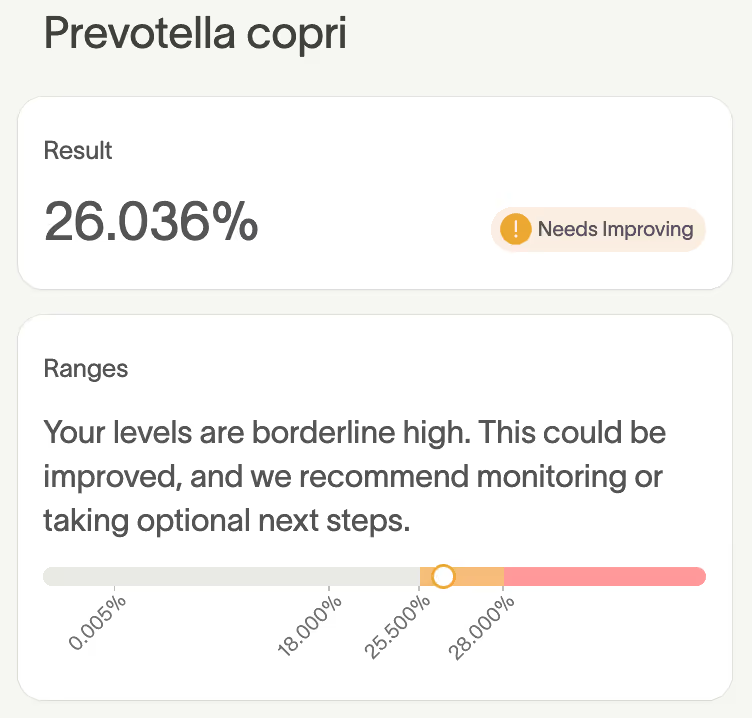
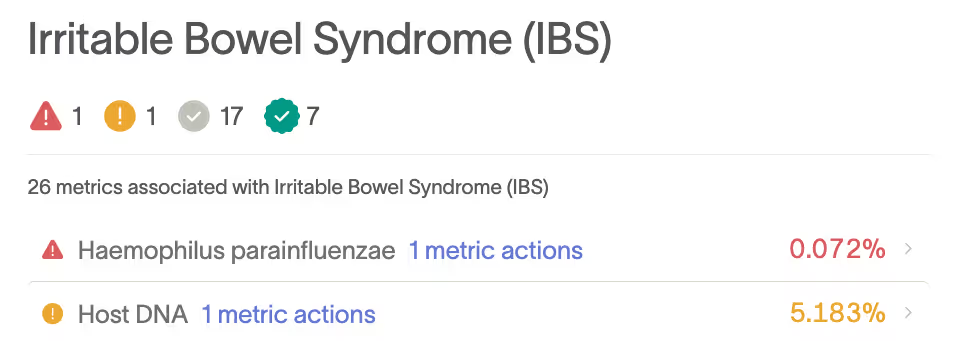
Her test showed an overgrowth of two microbes often seen in people with ulcerative colitis and Inflammatory Bowel Syndrome (IBS) — Haemophilus parainfluenzae and Prevotella copri [1]-[5]. Both are associated with gut inflammation, though their effects can vary depending on the specific strain and the overall environment.
Prevotella copri is one of the most common gut species. Beyond GI disorders, elevated levels have been linked to rheumatoid arthritis, insulin resistance, and diabetes [6]-[9].
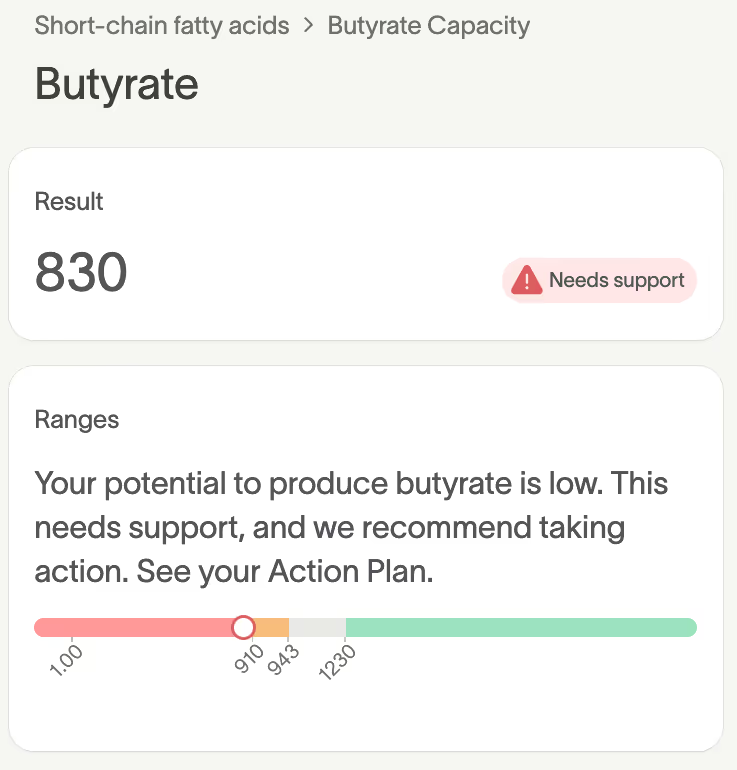
Carolyn’s butyrate production potential of 830 was also identified as needing support. Her gut bacteria had a reduced capacity to make butyrate, the main fuel for her intestinal lining cells.
Her test also revealed a host DNA level of 5.183%, marked as Needs Improving.
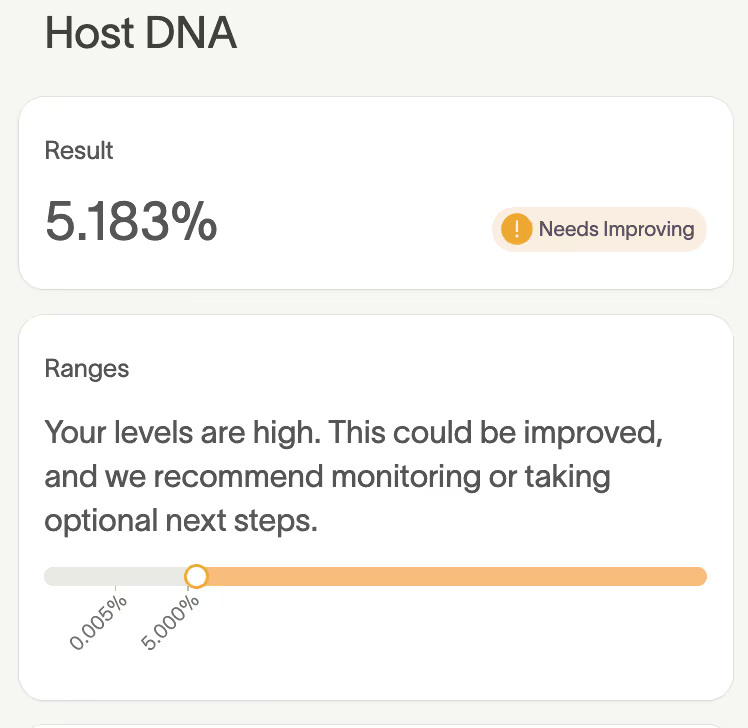
In the Adult Conditions & the Microbiome section of Carolyn's report, two metrics were flagged as potentially associated with IBS: Haemophilus parainfluenzae and Host DNA.
While no single microbe tells the whole story, patterns like these help practitioners pinpoint where inflammation and imbalance may begin.
For Carolyn, these results brought clarity. "It very much explained my colitis symptoms." After years of taking anti-inflammatory medications, she finally felt validated.
What followed was a carefully guided shift from simply treating symptoms to restoring balance.
A targeted Action Plan to address imbalances
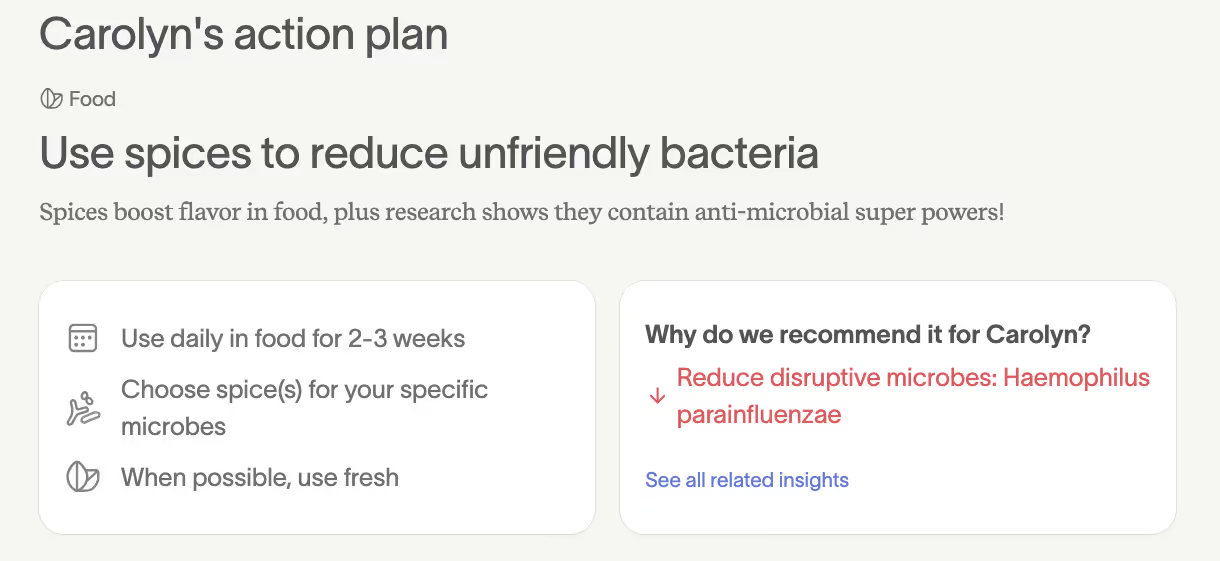
Working with her practitioner, Carolyn followed her personalized Action Plan and dug into the research behind her results to better understand them.
One of her first steps was adding spices to her diet to help reduce disruptive microbes and support beneficial ones. She started simply, adding cinnamon to her daily smoothies.
Carolyn also made strategic dietary shifts, cutting back on alcohol, gluten, dairy, and sugar, and began using the recommended probiotics.
"It was very simple to take the targeted probiotics; it was nice to know which strains to really focus on rather than just popping them at random."
What surprised her most was how manageable the changes felt. "It's almost maddening how easy it was to make some of these simple changes. I can't tell a difference in taste between the dairy-free kefir and the regular dairy I was eating. Sometimes I still miss cheese, but I'm still making good progress even with having the occasional dairy serving."
Over time, Carolyn noticed steady improvements. "My ulcerative colitis symptoms have resolved completely, and I'm off my anti-inflammatory medications, which is great." She was able to discontinue medications she thought she’d always have to take.
As her gut health stabilized, Carolyn and another integrative practitioner explored her broader stress response. Cortisol testing throughout the day revealed opportunities for support. By following recommendations to lower her cortisol — through daily cold showers (yes, she got used to them), temporary supplementation, and medication — her thyroid symptoms improved, too. Eventually, she was able to stop her thyroid medication as well.
Making changes to your health routine, especially adjusting medications or diet based on your microbiome test results, should always be done with guidance from a qualified healthcare professional, as Carolyn did. They know your complete health picture, so they can interpret your results and ensure your personalized Action Plan is safe, practical, and effective.
"I wish this were standard practice for everyone"

Looking back, Carolyn says her practitioner’s whole-body approach to health meant they were invested in uncovering the why behind her symptoms. And taking the gut health test was the tool that made it possible.
“It was very helpful, and I wish it were standard practice for everyone. It would help so many people cut down on healthcare expenses and get to the root cause of so many issues.”
Carolyn is no stranger to preventative approaches. Her son Edan was one of the first babies in the world diagnosed pre-symptomatically with spinal muscular atrophy (SMA), a genetic condition and the leading cause of infant death from genetic disease. Early testing through newborn screening and timely gene therapy intervention saved his life. “He is our miracle child, developing normally today," she shares.
Looking ahead, Carolyn hopes healthcare systems will one day embrace preventive gut health testing, covered by insurance, taught in medical schools, and used by doctors as part of routine care.
For anyone living with ulcerative colitis or ongoing digestive symptoms that haven’t been fully addressed through conventional care, a Gut Health Test can provide personalized insights to guide your next steps.
References
[1] D. M. Saulnier et al., “Gastrointestinal microbiome signatures of pediatric patients with irritable bowel syndrome,” Gastroenterology, vol. 141, no. 5, pp. 1782–1791, Nov. 2011, doi: 10.1053/j.gastro.2011.06.072.
[2] A. Lo Presti et al., “Fecal and Mucosal Microbiota Profiling in Irritable Bowel Syndrome and Inflammatory Bowel Disease,” Front Microbiol, vol. 10, p. 1655, 2019, doi: 10.3389/fmicb.2019.01655.
[3] M. Schirmer et al., “Compositional and Temporal Changes in the Gut Microbiome of Pediatric Ulcerative Colitis Patients Are Linked to Disease Course,” Cell Host Microbe, vol. 24, no. 4, pp. 600-610.e4, Oct. 2018, doi: 10.1016/j.chom.2
[4] X. Wang and H. Cao, “P090 Prevotella copri promotes colitis in mice by reducing expression of ATF4 and disturbing the gut microbiota,” J Crohns Colitis, vol. 18, no. Supplement_1, p. i364, Jan. 2024, doi: 10.1093/ecco-jcc/jjad212.0220.
[5] A. Lo Presti et al., “Phylogenetic analysis of Prevotella copri from fecal and mucosal microbiota of IBS and IBD patients,” Therap Adv Gastroenterol, vol. 16, p. 17562848221136328, Jan. 2023, doi: 10.1177/17562848221136328.
[6] A. Pianta et al., “Evidence of the Immune Relevance of Prevotella copri, a Gut Microbe, in Patients With Rheumatoid Arthritis,” Arthritis Rheumatol, vol. 69, no. 5, pp. 964–975, May 2017, doi: 10.1002/art.40003.
[7] J. U. Scher et al., “Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis,” Elife, vol. 2, p. e01202, Nov. 2013, doi: 10.7554/eLife.01202.
[8] H. K. Pedersen et al., “Human gut microbes impact host serum metabolome and insulin sensitivity,” Nature, vol. 535, no. 7612, pp. 376–381, July 2016, doi: 10.1038/nature18646.
[9] A. Z. Leite et al., “Detection of Increased Plasma Interleukin-6 Levels and Prevalence of Prevotella copri and Bacteroides vulgatus in the Feces of Type 2 Diabetes Patients,” Front Immunol, vol. 8, p. 1107, 2017, doi: 10.3389/fimmu.2017.01107.

