Shea*, an outgoing mom and part-time licensed marriage and family therapist, was facing the same challenges many of her clients did, navigating the ups and downs of perimenopause, along with the added challenge of Hashimoto’s and food intolerances.
She did what most of us would do: avoid the foods that triggered digestive issues. But it made family time less enjoyable and managing her symptoms felt like a job in itself.
Gut health wasn’t on Shea’s radar until a podcast sparked her curiosity about how it might relate to her own wellness path.
Now that her health is in a much better place, Shea is sharing her experience—what shifted, how she found support, and the gut testing that helped her rediscover her love of food and spontaneity.
The discomfort of living with food limitations
For years, Shea dealt with bloating, discomfort, and strict dietary restrictions tied to food intolerances and Hashimoto’s. Broccoli, corn, cheese, gluten—foods she once enjoyed—were off the table.
Shea tried the usual approach: avoiding anything that triggered symptoms, but restrictions made travel and family meals challenging, often requiring separate dinners for her.
Shea missed the everyday joy of sharing food with her loved ones. That disconnect stung.
“It was hard not being able to enjoy the same meals,” she said. “I didn’t want to be the reason we couldn’t go to certain restaurants.”
The endless loop of looking for answers and managing her symptoms drained her energy. Then, while listening to the Holding Space podcast, Shea heard our founder, Cheryl Sew Hoy, explain how gut imbalances are often the root cause of many symptoms. That message resonated and became the catalyst for Shea’s first gut health test.
What followed was anything but linear: a zigzag of progress, setbacks, and a throughline of resilience.
A year and four tests in
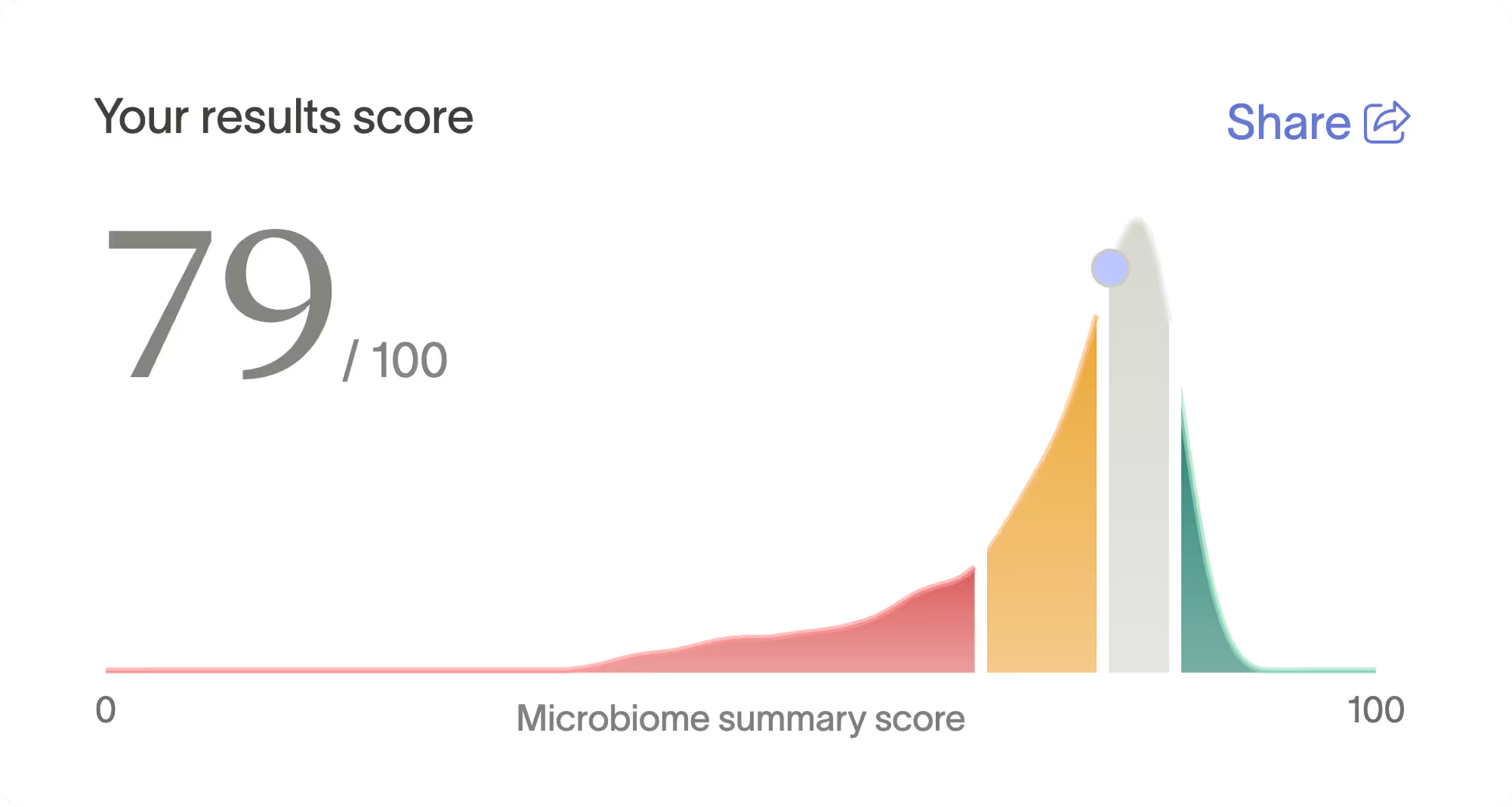
After surgery, an ear infection, and a round of antibiotics, Shea’s Microbiome Summary Score showed her gut was out of balance.
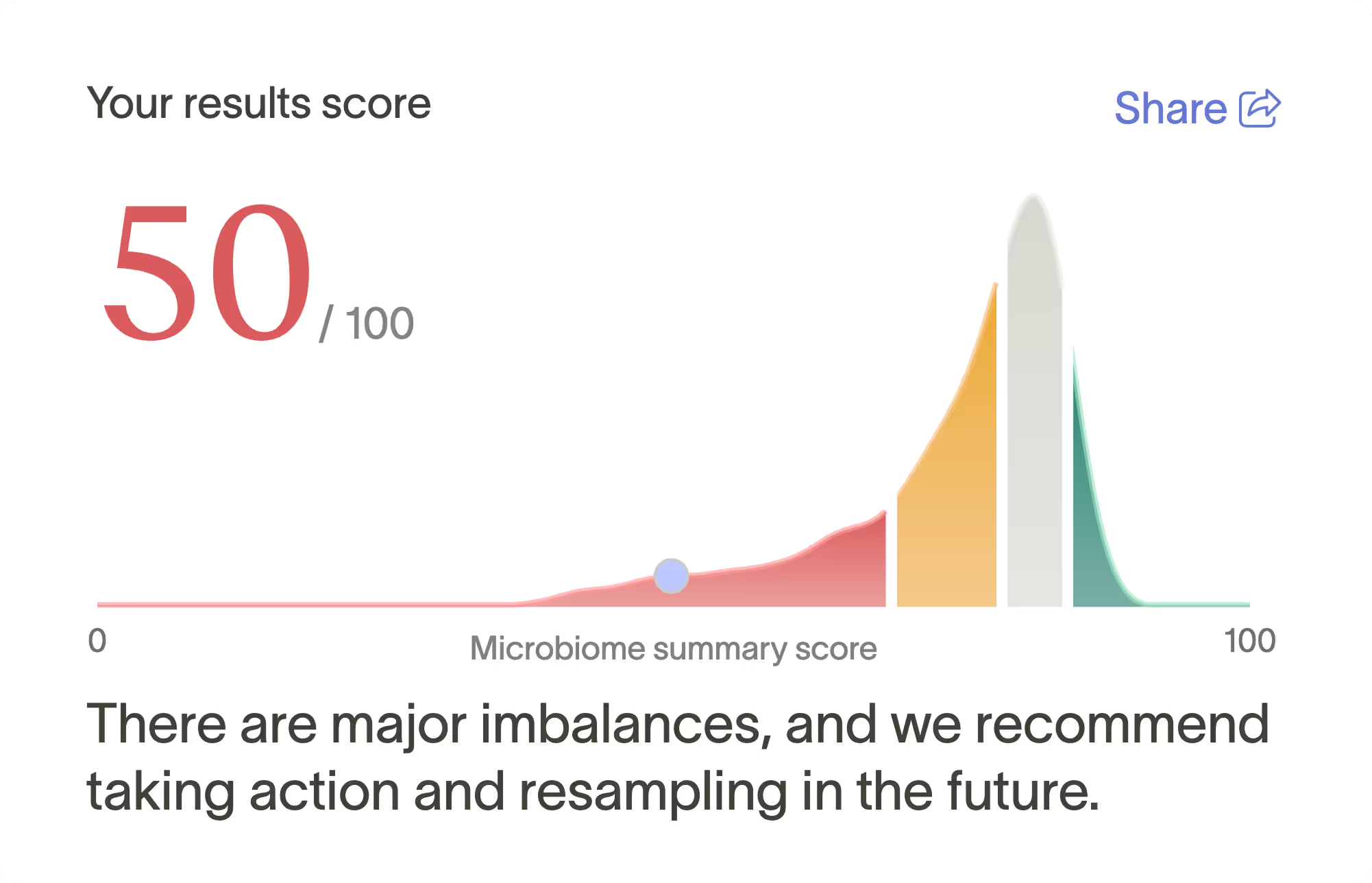
Guided by her Action Plan, she followed the recommended steps. A few months later, she retested and saw impressive improvements.
In her earlier test this year, the area that needed the most support was Shea’s gut inflammation markers.
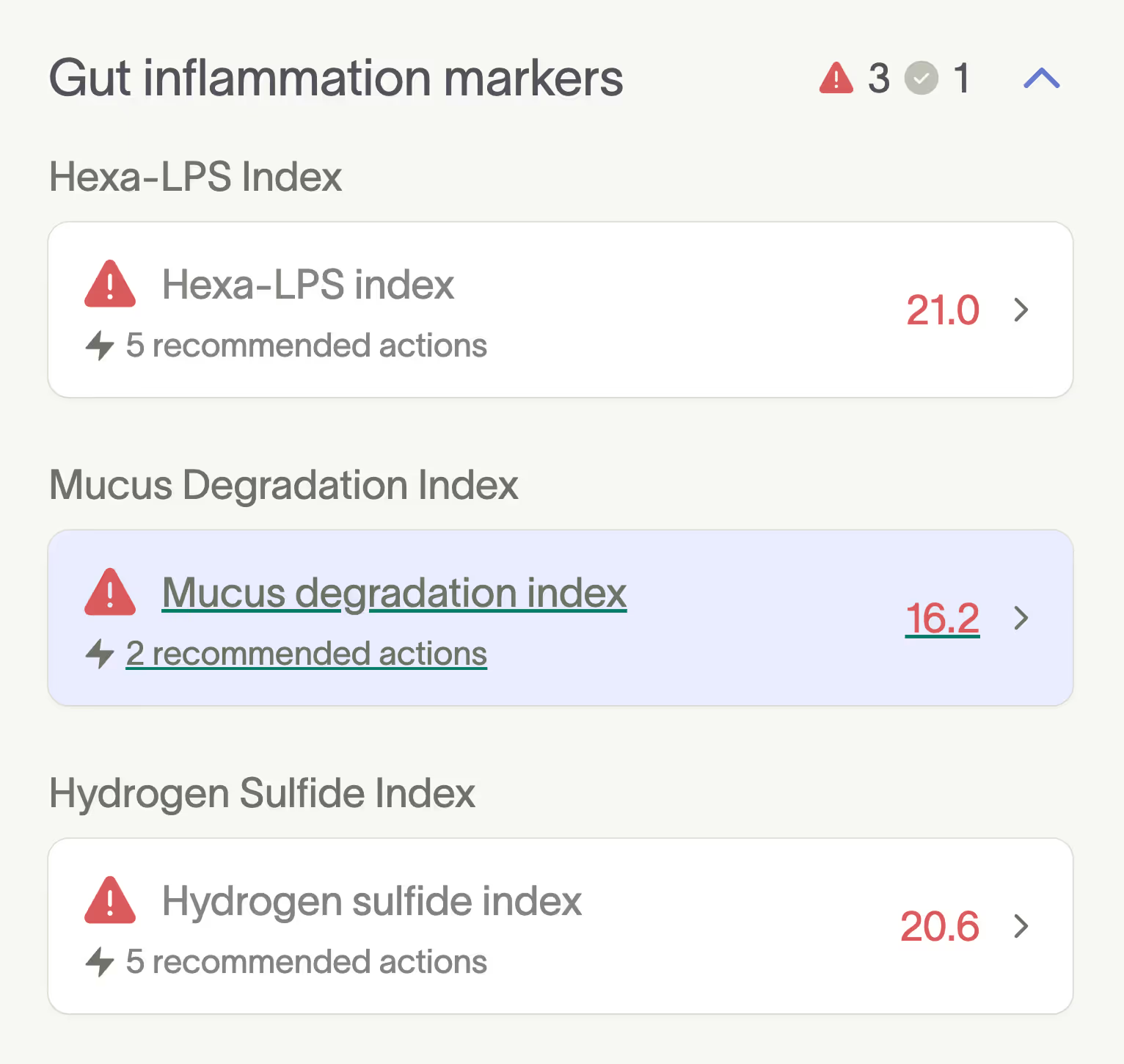
All three of these metrics give insight into how well your gut barrier is functioning and whether your microbiome is contributing to or protecting against inflammation. Elevated levels suggest Shea’s gut is under stress, and that targeted support could help restore balance.
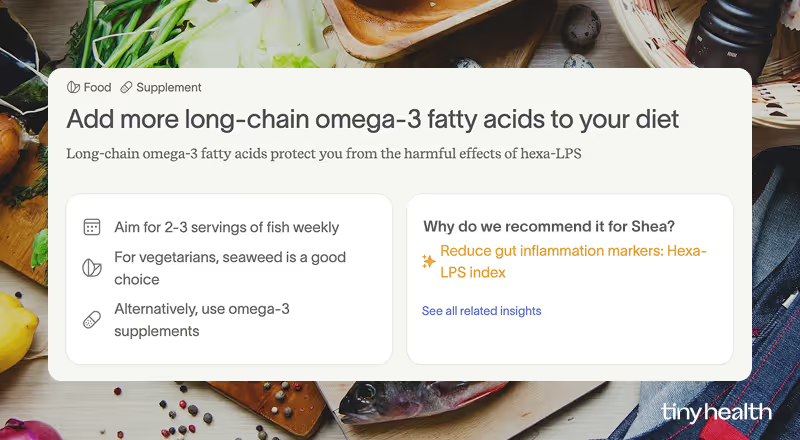
Each flagged metric included a recommendation for course correction, like this one to improve her hexa-LPS index.
When Shea retested, her gut inflammation markers had either normalized or entered the optimal range, indicating that she’d been consistently following the steps in her Action Plan.

Shea’s initial results also revealed low butyrate production. This key short-chain fatty acid helps strengthen the gut lining, reduce inflammation throughout the body, and support immune function and energy metabolism [1]. Getting this into a healthy range will help Shea bounce back from gut disruptions, like antibiotics.

Targeted recommendations to help her gut naturally produce more butyrate included taking a butyrate supplement, a Bacillus probiotic, and adding more fibers like inulin and resistant starch to her diet. Notice the clear shift in her resample; Shea’s butyrate capacity, once below healthy levels, is now in the normal range.
Shea's gut type was classified as Enterobacteriaceae earlier this year, indicating she had elevated levels of disruptive bacteria, like Escherichia coli and Klebsiella, which can cause digestive issues and inflammation [2], [3].
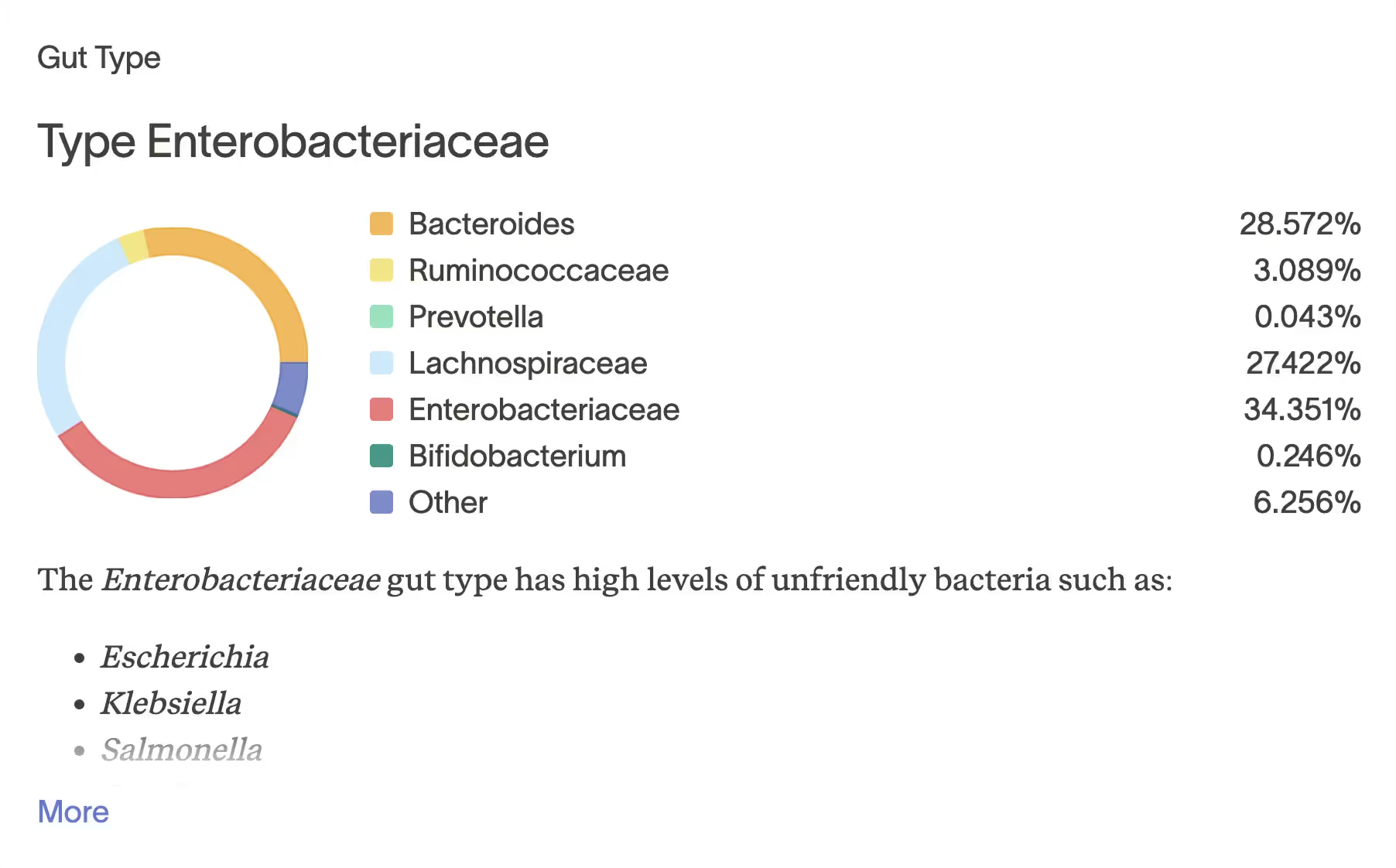
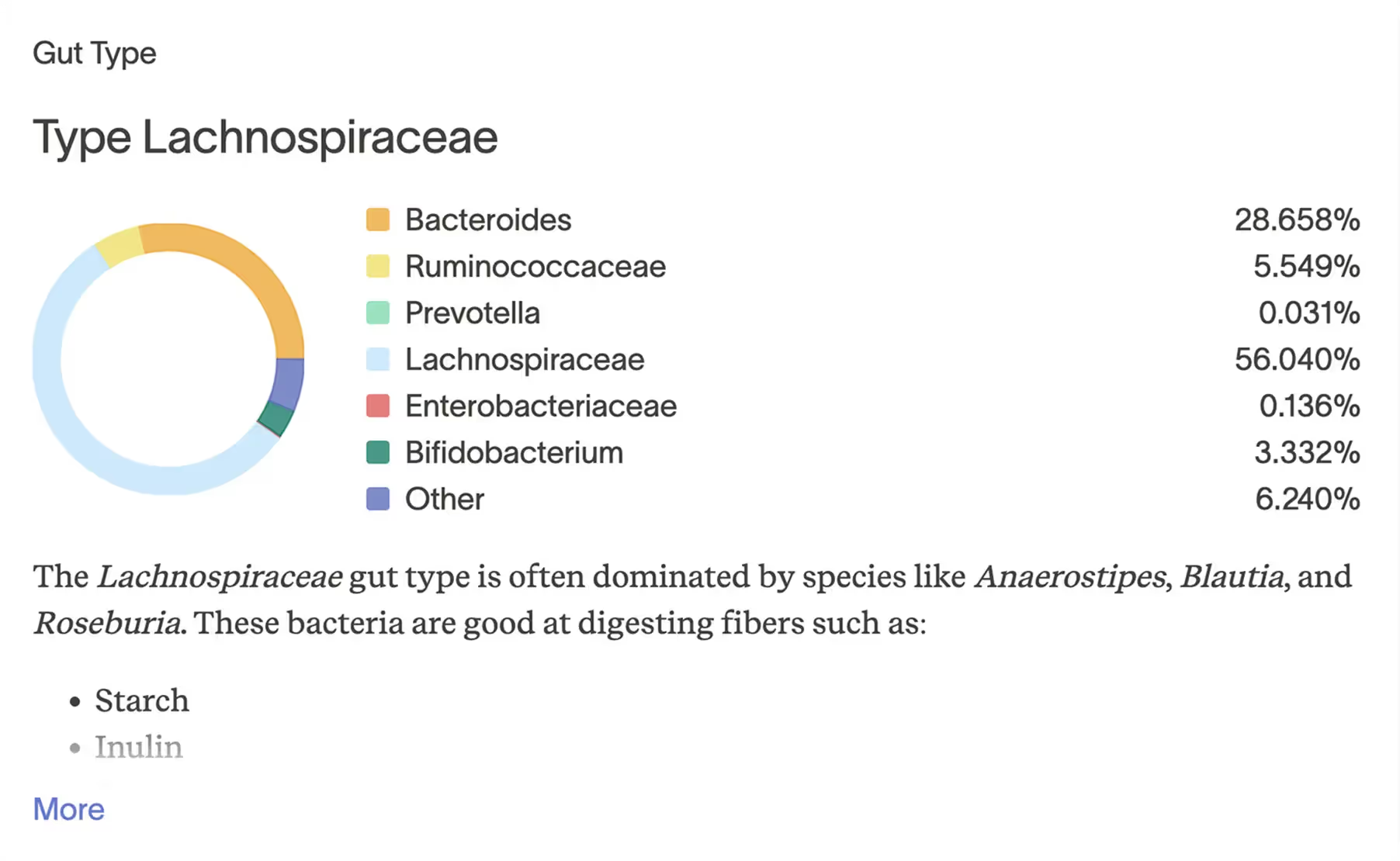
Shea’s most recent test shows that beneficial bacteria now dominate her gut composition. Notice how the disruptive species Enterobacteriaceae dropped from 34.351% to 0.136%, a 99.6% decrease. Another improvement, her Bifidobacterium levels rose from just 0.246% to 3.332%—a more than 13-fold increase. That’s important because Bifidobacteria play a crucial role in digestion, immune support, and maintaining a balanced microbiome [4]. Together, these results reflect a meaningful shift: Shea’s gut is much more resilient and balanced.
How she did it: Shea’s plan + microbiome support
Shea’s Action Plan included targeted prebiotics and probiotics, along with food and lifestyle recommendations that supported specific things in her results.
She also had Amy Orlandi, her microbiome specialist, to guide her through the process. “She was amazing—helpful, supportive, and she answered every question I had,” Shea said.
At first, she wanted to try everything at once, especially product recommendations. “I probably spent too much money right away,” Shea laughed. But the step-by-step plan helped her stay focused on what mattered most. The steady changes she made to her routine paid off. Her symptoms were getting better.
Shea learned something with every test. The biggest takeaway? Her microbiome was highly reactive, shifting in response to positive changes and unexpected setbacks. A lot can happen in a year. For Shea, that meant antibiotics, surgery, and food poisoning, the kinds of disruptions that can throw your gut off balance. But seeing her results felt empowering. When her scores dipped, she returned to her Action Plan and made adjustments. Each time, her gut bounced back, a sign of its resilience.
For Amy, working with someone excited to make changes was fulfilling. “I remember Shea telling me that all she wanted to do was enjoy tacos again. I often tell people that setbacks will occur along the way. Balancing the microbiome isn’t a linear process; it’s more than just taking a probiotic. It often involves small but impactful changes over time,” Amy said.
What's possible now
Shea's symptoms no longer dictate what she eats and where she dines with her family. “Pass the tacos” is back in dinner conversation, along with the spontaneity of trying once-off-limits foods during family outings.
Corn, broccoli, dairy, gluten, all the foods she used to avoid, are back on the menu in moderation. No more bloating. No more dread before a meal.
“I can go anywhere and not be limited,” she said. “That’s very freeing for me.”
After years of managing symptoms, Shea inspired her family to prioritize their wellness. Now her son's gut health test is on the way, and her husband is up next. “I just want to be in the best health I can be,” she said.
If you relate to Shea’s story, our Adult Gut Health Test offers a measurable way to take charge of your well-being.
*Our customer gave us permission to share her story and photo, but we've used an alias to protect her privacy.


