For millions of people around the world, alcohol is an accepted part of their diet. Especially during the holidays, when the number of people reported to drink alcohol doubles [1]. But is alcohol consumption "good" for your health? And is alcohol bad for gut health? The answer is complex.
Whether alcohol consumption is good or bad for you depends on various factors. These include:
- How much alcohol is consumed;
- The type of alcohol consumed;
- Individual health conditions; and
- Overall lifestyle [2].
The potential benefits of alcohol are often associated with moderate and responsible consumption. And excessive drinking can have serious health consequences [2], [3]. While alcohol is widely consumed for its social and cultural appeal, let's delve deeper into how it interacts with your body. In this post we'll answer the question, does alcohol kill gut bacteria? And we’ll discuss the relationship between alcohol and gut health, a key player in your overall health and wellness.
Alcohol and the Gut Microbiome
Did you know that your gut microbiome, a bustling community of microorganisms in your digestive system, holds the key to numerous health benefits? From nutrient absorption to immune strength, maintaining a balanced and diverse gut microbiome is crucial for your overall health. But this delicate balance can be disrupted by alcohol, leading to issues like inflammation and dysbiosis—a state of imbalance [4].
This begs the question, does alcohol kill good gut bacteria? And how does drinking impact the delicate balance of beneficial and unfriendly bacteria in your gut microbiome? First, the concentration of alcohol needed to kill bacteria, around 70%, far exceeds the alcohol content of most beverages, especially after mixing with everything else in your body. So a regular drink won’t sterilize your gut microbiome. However, prolonged and excessive alcohol consumption can have negative effects on the microbiome. Keep reading to explore the many impacts of alcohol on the gut.
Dysbiosis and reduced butyrate production.
Scientific studies suggest that alcohol consumption triggers changes in the gut microbiota. This can lead to imbalances in the gut microbiome, known as dysbiosis. These shifts can involve:
- A decrease in beneficial bacteria like Akkermansia, Roseburia, Faecalibacterium, and Bacteroides
- Reduced production of butyrate—a vital compound to maintain intestine balance, and
- An overabundance of Gammaproteobacteria and related opportunistic pathogens [5].
Increased intestinal permeability
The intestinal barrier controls what can pass between the gastrointestinal tract and the bloodstream. It allows nutrients to be absorbed and prevents harmful substances from entering the bloodstream. This barrier is made of water, mucous gel, and epithelial and connective tissue. Studies suggest individuals with a history of alcohol abuse may have a weakened intestinal barrier. When this happens, unwanted substances, including microbes, can enter the bloodstream [6].
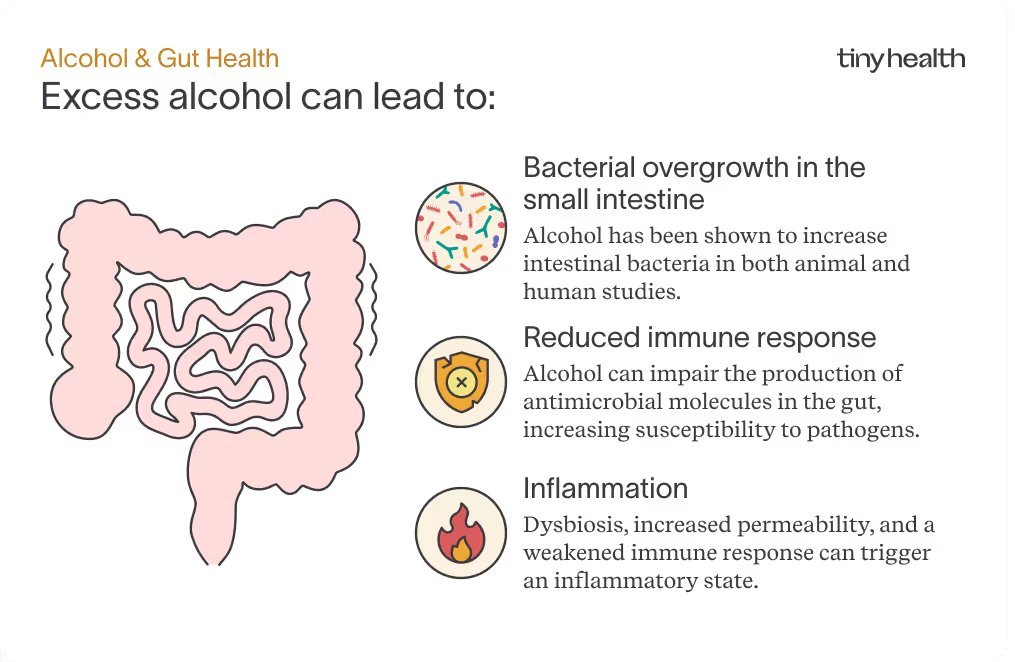
Excess alcohol can lead to:
- Bacterial overgrowth in the small intestine. Alcohol has been shown to increase intestinal bacteria in both animal and human studies [6].
- Reduced immune response. Alcohol can impact the production of antimicrobial molecules in the gut. This increases your susceptibility to intestinal pathogens [6].
- Inflammation. Dysbiosis, increased permeability, and a lower immune response can promote an inflammatory response [6].
Potential benefits of moderate alcohol consumption
While plenty of evidence shows that too much alcohol can have negative impacts on your health, studies have also linked alcohol consumption to some benefits.
- Social and psychological aspects. Moderate alcohol consumption is often a part of social and cultural activities, and for many people, it can contribute to relaxation and enjoyment.
- Longevity. Some research indicates that moderate alcohol consumption may be linked to increased longevity. That said, the mechanisms behind this association are not fully understood [7], [8].
- Increase in beneficial bacteria. A study linked an increase of beneficial bacteria in humans to consumption of polyphenols—antioxidant molecules found in tea, red wine, coffee, and olive oil [9].
Defining Moderate vs. Excessive Alcohol Consumption
While moderate alcohol consumption may offer some benefits for the microbiome and overall health, it's important to strike a balance.
A low-risk level of consumption is defined by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) as follows:
- No more than 3 drinks on any single day and no more than 7 drinks per week for women
- No more than 4 drinks on any single day and no more than 14 drinks per week for men.
The Dietary Guidelines for Americans, on the other hand, define moderate drinking as up to 1 drink per day for women and up to 2 drinks per day for men. In the US, a standard drink is defined as a drink with 14 grams (0.6 fluid ounces) of pure alcohol. This equates to:
- 12 ounces of regular beer, which is usually about 5% alcohol
- 5 ounces of wine, which is typically about 12% alcohol
- 1.5 ounces of distilled spirits, which is about 40% alcohol
So what is considered excessive drinking?
- Binge drinking: 4 drinks (women) or 5 drinks (men) in a 2-hour time frame.
- Extreme binge drinking: 8 drinks or more (women) or 10 drinks or more (men).
- Heavy drinking: Binge drinking 5 or more days in the past 30 days.
But how does alcohol affect your gut health? The truth is, it can have detrimental effects on the delicate ecosystem of the gut microbiome, leading to a cascade of health issues. As research in this field continues to evolve, you should make informed choices about alcohol consumption. Consider both the potential benefits and drawbacks for your overall well-being. Ultimately, moderation remains key to maintaining a healthy relationship between the microbiome and alcohol.
How to Restore Gut Health After Alcohol Consumption
If you’re worried about your gut health after consuming alcohol, we have good news. By adopting better habits and dietary choices, you can help restore the gut microbiome and mitigate potential damage caused by alcohol. Here are some strategies to support your gut after consuming alcohol:
- Stay hydrated or use electrolyte supplements to support fluid balance, muscle, and nerve function. Alcohol can cause dehydration, so drinking plenty of water or using electrolyte-rich supplements is essential for rehydration.
- Consume probiotics. Probiotics found in fermented foods like yogurt, kefir, sauerkraut, kimchi, and over-the-counter probiotic supplements can help restore gut balance.
- Include prebiotics in your diet. Foods like garlic, onions, leeks, bananas, asparagus, and whole grains can nourish beneficial gut bacteria.
- Increase fiber-rich foods. Fruits, vegetables, whole grains, and legumes help to promote gut health by supporting the growth of beneficial bacteria.
- Opt for anti-inflammatory foods. Fatty fish, nuts, seeds, and colorful fruits and vegetables can counteract the inflammation caused by alcohol consumption.
- Avoid over-the-counter pain relievers. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can irritate the stomach lining when combined with alcohol.
- Prioritize rest. Alcohol disrupts your sleep patterns. Adequate sleep is crucial for overall health, including gut health.
Taking a break from drinking alcohol
Another idea to consider is scaling back your alcohol consumption, or taking a break from alcohol altogether. Take, for example, a recent study of people with alcohol use disorder who had high intestinal permeability. In the study, a 3-week abstinence from alcohol resulted in a complete recovery of the subjects’ gut barrier function [10]. This shows the strong link between gut health and alcohol, and how moderation is important.
You may have also heard of Dry January, an annual trend that started in the UK several years back. What is Dry January? It’s a challenge where people abstain from alcohol all January to give their bodies a reset and form healthier habits.
Many people experience great benefits from this month off from alcohol, such as better sleep, more energy, better skin and hair, and weight loss [11]. In a survey of over 4,000 adults who participated in Dry January, every single respondent reported an increase in their well-being and their self-efficacy—their belief that they could reach their goals [12].
Conclusion: Balancing Alcohol and Gut Health
While alcohol may offer some health benefits in moderation, it's crucial to be aware of its complex effects on the gut microbiome. Alcohol can disrupt the delicate balance of microorganisms in the gut, leading to dysbiosis, increased intestinal permeability, and other health issues. Following moderate consumption guidelines can help reduce these health risks.
After alcohol consumption, you can support your gut health through hydration, probiotics, prebiotics, fiber-rich foods, and proper rest. Even a brief period of abstinence from alcohol may be beneficial to help restore your gut. Remember, moderation and informed choices are key to maintaining a healthy gut microbiome and your overall well-being.
If you are experiencing persistent digestive issues, please consult with your medical provider. To check for gut imbalances and get a personalized plan to optimize your microbiome, try an Adult Gut Health Test from Tiny Health today.
Note: Not all individuals who drink alcohol experience the same effects, nor will everyone develop an alcohol use disorder. But if you are concerned about your drinking habits or those of someone you love, help is available. In the U.S., FindTreatment.gov is a confidential and anonymous resource that can help you find the support you need.


