A Tiny Health study observed that among adults aged 30–40, light drinkers had higher levels of beneficial gut bacteria compared to non-drinkers, while heavy drinkers showed higher levels of bacteria associated with inflammation and gut barrier stress, also compared to non-drinkers. Findings suggest moderation and healthy lifestyle habits support gut balance.
How Light and Heavy Drinking Habits Impact Your Gut Microbiome

Summary
For many, alcohol is a staple of our social life, whether it's an occasional happy hour with colleagues or weekend drinks with friends. But its impact on the body, including the gut microbiome, depends on several factors: amount, frequency, and your unique biology.
We analyzed survey responses alongside gut microbiome profiles from over 2,000 adults aged 30–40 in our community who had completed a Tiny Health Gut Health Test and lifestyle questionnaire. Participants were grouped from teetotalers to heavy drinkers to uncover patterns showing how alcohol intake is associated with shifts in gut microbes.
Our findings don’t prove cause and effect, but they do offer valuable clues about alcohol’s role in microbiome balance.
How we classified drinking habits
To make sense of what we found, we looked at how our community members described their alcohol drinking habits and organized them into two categories:
- Light drinkers: People who enjoy alcohol occasionally but stay below what researchers consider heavy drinking
- Heavy drinkers: Those whose drinking habits exceeds recommended limits
We chose these classifications because science consistently shows that alcohol's effects on gut health—and our bodies—depend on amount and frequency [1], [2]. It's also the same approach that public health experts use when studying drinking patterns.
Generally, light to moderate drinking is often defined as two drinks or less per day for men and one drink or less per day for women. Heavy drinking is classified as having more than four drinks a day (more than fourteen drinks per week) for men, and more than three drinks a day (more than seven drinks per week) for women [3].
Our survey looked at how often and how much people drink—but not what they drink. So whether it’s wine, beer, or cocktails, our results speak to overall drinking patterns, not how specific beverages might affect the gut.
It’s also worth noting that light and heavy drinkers often differ in other lifestyle habits too, like diet and exercise, which can also shape the microbiome alongside alcohol use [4].
Key bacterial shifts that emerged
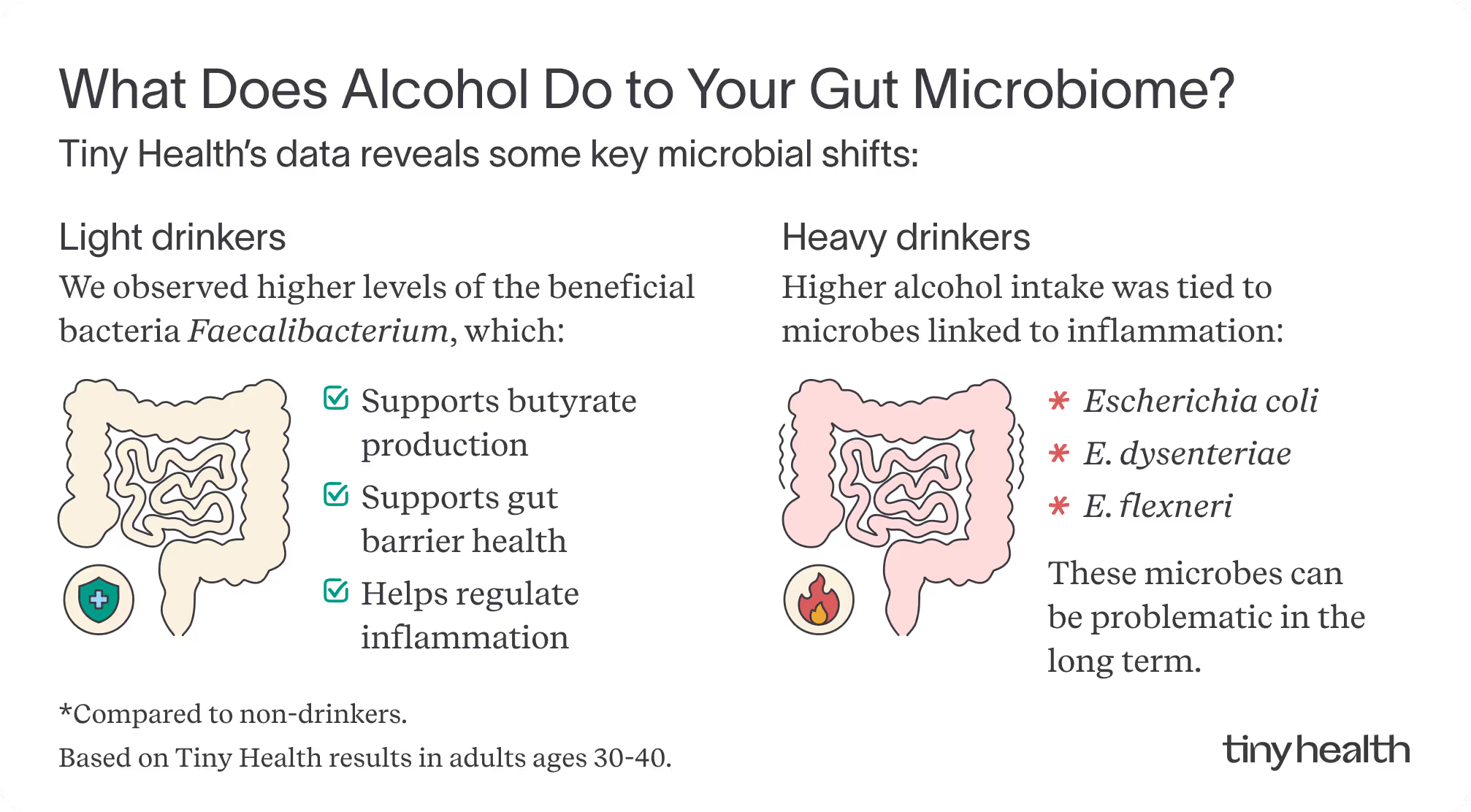
Our data infographic illustrates the relationship between gut composition and the presence of specific microbes in individuals who are light and heavy drinkers.
Key bacterial shifts that emerged:
Gut health effects of light drinking
Those who fall into this category show a trend toward higher levels of Faecalibacterium, compared to non-drinkers. Faecalibacterium, a beneficial gut bacterium, is linked to butyrate production, gut barrier support, and regulation of inflammation [5], [6]. While these findings suggest microbial differences associated with drinking patterns, the health associations are linked to Faecalibacterium itself, rather than alcohol consumption.
Gut health effects of heavy drinking
In contrast to non-drinkers, those who drink heavily show higher levels of bacteria associated with gut barrier stress and inflammation, including Enterobacteriaceae, such as Escherichia coli, than non-drinkers. While Escherichia coli and other Enterobacteriaceae bacteria are common in the gut, some strains can stress the gut lining. Higher levels of E. coli and similar microbes have been linked to chronic inflammation, liver disease, and metabolic disorders, such as insulin resistance [7].
Key functional changes
In addition to how alcohol alters the presence of microbes in your gut, our data also highlights how they function.

Notice how heavy drinking is associated with an increase in lipopolysaccharide (LPS) production, a compound produced by certain Gram-negative bacteria that can cross a weakened gut lining, triggering immune responses and fueling chronic inflammation [8].
Hydrogen sulfide (H₂S) can be a protective gut signal that supports blood flow, repairs tissue, and calms inflammation. But when epithelial defenses are weakened or bacterial production is excessive, it can overwhelm detox systems and irritate or damage the gut lining [9].
Another shift involves GABA degradation, which reduces the availability of this calming neurotransmitter and potentially affects gut–brain communication [10].
Together, these functional shifts suggest that alcohol has the potential to alter microbial behavior and create conditions that could be linked to both gut and systemic health issues.
What grabbing a drink means for your gut
These findings raise interesting questions about how alcohol shapes your gut. The patterns we discovered align with research that says drinking in moderation may support a relatively balanced microbiome. In contrast, the microbiome activity observed in individuals who heavily drink is associated with reduced resilience.
Light drinkers may have other lifestyle habits, such as a healthy diet, that create an ideal environment for beneficial microbes like Faecalibacterium to thrive. Meanwhile, heavy drinking is associated with shifts in the gut, potentially increasing intestinal permeability and changing nutrient availability in ways that favor inflammatory bacteria.
Your gut bacteria are constantly reacting to your diet, stress levels, sleep quality, workout routines, and any medications you take [11], [12]. So, while these drinking patterns reveal important insights, they likely reflect the complexity of many other factors beyond what's in someone's glass.
Connecting the dots
Your gut is home to trillions of microbes that thrive when they are in balance. Alcohol is one factor that can shift this delicate ecosystem. When you stick to lighter drinking, you’re more likely to support a gut environment linked to resilience and lower inflammation.
And when that intention extends to other healthy habits, such as getting quality sleep, eating nutrient-dense foods, and managing stress, it creates the conditions for better digestion, immunity, and overall well-being.
Wondering if your drinking habits are affecting your gut? An Adult Gut Health Test provides clear insights by measuring gut inflammation markers and microbial diversity, along with personalized recommendations to optimize your well-being.

Trust your gut.
References
[1] G. Chiva-Blanch and L. Badimon, “Benefits and Risks of Moderate Alcohol Consumption on Cardiovascular Disease: Current Findings and Controversies,” Nutrients, vol. 12, no. 1, p. 108, Dec. 2019, doi: 10.3390/nu12010108.
[2] K. J. Biddinger et al., “Association of Habitual Alcohol Intake With Risk of Cardiovascular Disease,” JAMA Netw Open, vol. 5, no. 3, p. e223849, Mar. 2022, doi: 10.1001/jamanetworkopen.2022.3849.
[3] Y.-J. Choi, S.-K. Myung, and J.-H. Lee, “Light Alcohol Drinking and Risk of Cancer: A Meta-Analysis of Cohort Studies,” Cancer Res Treat, vol. 50, no. 2, pp. 474–487, Apr. 2018, doi: 10.4143/crt.2017.094.
[4] R. Lin et al., “The effects of cigarettes and alcohol on intestinal microbiota in healthy men,” J Microbiol., vol. 58, no. 11, pp. 926–937, Nov. 2020, doi: 10.1007/s12275-020-0006-7.
[5] K. Hodgkinson et al., “Butyrate’s role in human health and the current progress towards its clinical application to treat gastrointestinal disease,” Clinical Nutrition, vol. 42, no. 2, pp. 61–75, Feb. 2023, doi: 10.1016/j.clnu.2022.10.024.
[6] R. Martín et al., “Faecalibacterium: a bacterial genus with promising human health applications,” FEMS Microbiol Rev, vol. 47, no. 4, p. fuad039, July 2023, doi: 10.1093/femsre/fuad039.
[7] F. Di Vincenzo, A. Del Gaudio, V. Petito, L. R. Lopetuso, and F. Scaldaferri, “Gut microbiota, intestinal permeability, and systemic inflammation: a narrative review,” Intern Emerg Med, vol. 19, no. 2, pp. 275–293, Mar. 2024, doi: 10.1007/s11739-023-03374-w.
[8] A. Farhana and Y. S. Khan, “Biochemistry, Lipopolysaccharide,” in StatPearls, Treasure Island (FL): StatPearls Publishing, 2025. Accessed: Sept. 26, 2025. [Online]. Available: http://www.ncbi.nlm.nih.gov/books/NBK554414/
[9] A. G. Buret, T. Allain, J.-P. Motta, and J. L. Wallace, “Effects of Hydrogen Sulfide on the Microbiome: From Toxicity to Therapy,” Antioxidants & Redox Signaling, vol. 36, no. 4–6, pp. 211–219, Feb. 2022, doi: 10.1089/ars.2021.0004.
[10] P. Strandwitz et al., “GABA Modulating Bacteria of the Human Gut Microbiota,” Nat Microbiol, vol. 4, no. 3, pp. 396–403, Mar. 2019, doi: 10.1038/s41564-018-0307-3.
[11] Y. Yang, M. C. Hernandez, S. Chitre, and C. Jobin, “Emerging roles of modern lifestyle factors in microbiome stability and functionality,” Curr. Clin. Microbiol. Rep., vol. 12, no. 1, pp. 1–11, Mar. 2025, doi: 10.1007/s40588-025-00242-3.
[12] M. Van Hul, P. D. Cani, C. Petitfils, W. M. De Vos, H. Tilg, and E. M. El-Omar, “What defines a healthy gut microbiome?,” Gut, vol. 73, no. 11, pp. 1893–1908, Oct. 2024, doi: 10.1136/gutjnl-2024-333378.

