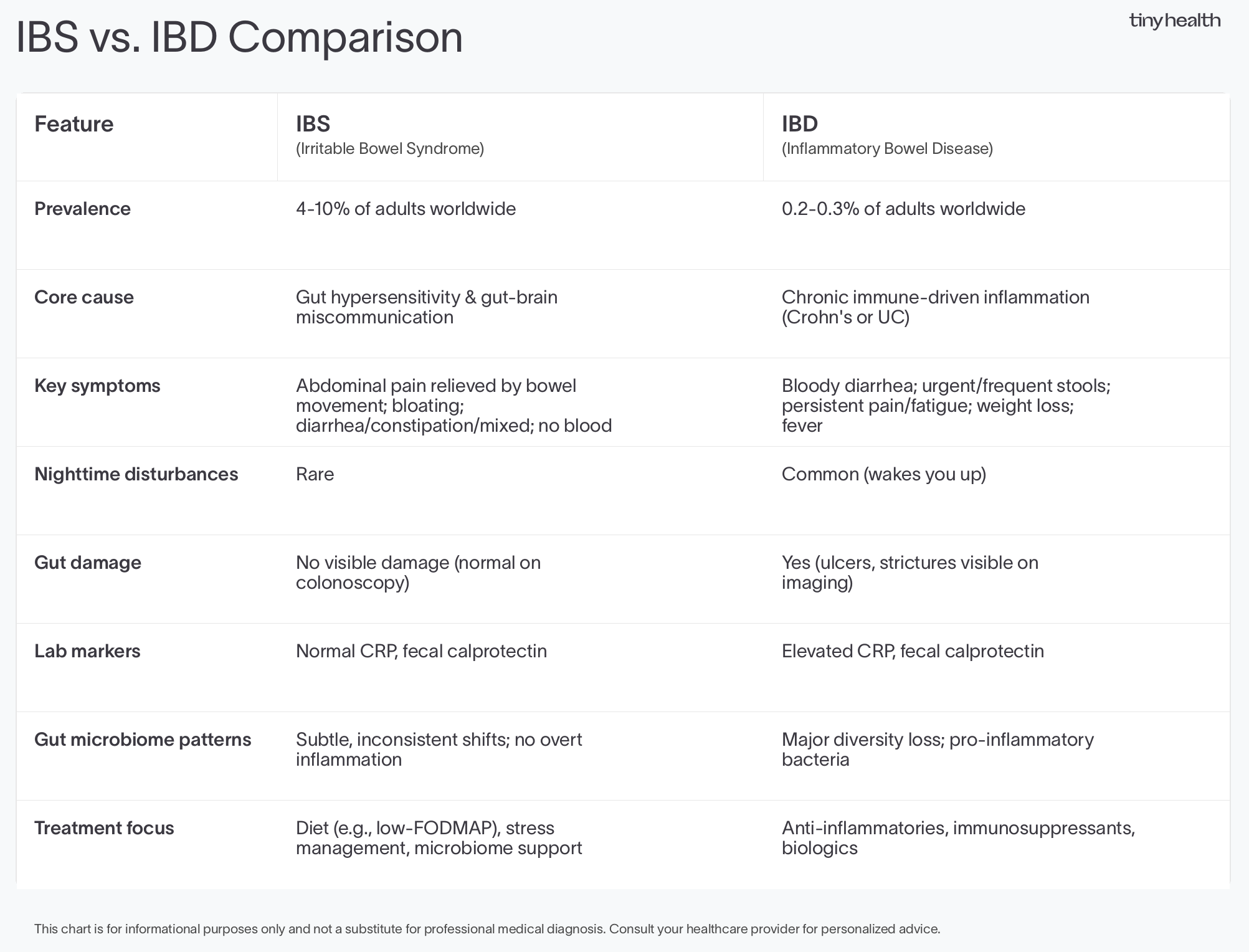
IBS and IBD share symptoms like stomach pain and bloating, but they have different causes. IBS stems from gut-brain miscommunication, while IBD involves chronic immune-driven inflammation that can damage the digestive tract. Learn the distinct symptoms of each condition, how gut bacteria affect them differently, and get a side-by-side comparison chart to quickly spot what makes them unique.
IBS vs IBD: What's the Difference and Why It Matters

Summary
Stomach pain, bloating, and unpredictable bathroom trips. Symptoms that flare when stress hits. A gut that feels like it's running your life.
If these sound familiar, you may be living with irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD).
The names are alike, and the symptoms sometimes overlap. But each has distinct origins and treatments. One condition stems from gut hypersensitivity, the other from chronic immune-driven inflammation.
In this article, we'll cover what each disorder is, the role your microbiome plays, and why getting the right diagnosis matters for long-term health.
IBS and IBD explained
Some symptoms of IBS and IBD are similar, but the root causes are entirely different. IBS is about sensitivity. IBD is about inflammation.
IBS: When your gut becomes overly sensitive
If you have IBS, you're among the 4 to 10 percent of adults worldwide with this condition [1]. And you probably experience stomach pain, gas, bloating, and unpredictable bowel movements [2]. IBS is a gut-brain communication disorder, meaning your gut and nervous system aren't communicating the way they should.
IBS develops when your gut becomes more reactive than usual, and the signals between your gut, immune system, bacteria, and brain get crossed [3], [4]. This affects:
- How intensely you feel pain signals
- How quickly food moves through your digestive system
- How your gut reacts to stress
- How bacteria interact with your gut lining
Some people develop post-infectious irritable bowel syndrome after food poisoning or a stomach bug. The infection clears, but your gut remains hypersensitive.
Doctors diagnose IBS based on your symptoms after ruling out other possibilities like IBD [4]. Unlike IBD, your gut lining usually looks normal on imaging scans. It doesn’t show the kind of inflammation or tissue damage seen in IBD [3], [4]. Also, IBS isn’t linked to higher mortality rates or progressive damage to the gut [3].
IBS is categorized by your main symptom pattern. You might have IBS-D (diarrhea-predominant), IBS-C (constipation-predominant), or mixed type. Treatment focuses on finding relief through diet adjustments, such as a 30-day IBS diet plan, microbiome support, and approaches that calm the gut-brain connection [2].
IBD: When your immune system gets confused
If you have IBD, you're among the 0.2 to 0.3 percent of adults worldwide living with this condition [5].
Chronic inflammation of the GI tract (gastrointestinal tract) drives IBD, which includes Crohn's disease and ulcerative colitis [6], [7]. Both involve your immune system, which mistakenly targets your gut lining, causing inflammation, tissue injury, and sometimes lasting structural changes (i.e., narrowing of the intestine) that may affect how your digestive system works.
Crohn's disease can develop anywhere in your digestive system. The inflammation reaches deep into your intestinal wall. Ulcerative colitis only affects your colon, where inflammation spreads across the inner lining, creating ulcers.
If you have IBD, you might experience:
- Diarrhea, sometimes with blood
- Stomach pain
- Persistent fatigue that doesn't ease with rest
- Urgent bathroom trips
- Unintended weight loss or reduced appetite
Because inflammation affects your whole body, IBD can show up in other ways, too. In fact, up to 40 percent of those diagnosed experience symptoms beyond the gut [3]. Your joints may ache, your eyes may become irritated, or you may develop skin issues or liver concerns.
Getting diagnosed with IBD usually involves several steps [7], [8]:
- Colonoscopy and biopsies so your doctor can see inflammation directly
- Blood and stool tests, including fecal calprotectin, a measure of gut inflammation levels that's trackable in our Pro Gut Health Test (available through your practitioner)
- Blood tests that measure inflammatory proteins help doctors distinguish between ulcerative colitis and IBS, despite their shared symptoms.
- Imaging scans are used when your doctor needs to examine deeper areas of your digestive tract
IBD tends to cycle between flares and remission. During flares, your symptoms worsen. During remission, things calm down. Treatment focuses on managing your immune response. Your practitioner might recommend medications that reduce inflammation, suppress your immune response, or block specific signals that trigger flares.
IBS vs IBD symptoms difference
Here’s a closer look at distinctive symptoms and patterns that point doctors toward the right diagnosis.
Blood in your stool is one of the clearest differences. With IBD, you might notice blood when you have diarrhea. The inflammation is severe enough to cause bleeding in the lining of your gut. With IBS, blood is rare. If you're experiencing IBS symptoms and suddenly see blood, your doctor will likely investigate what's happening [7].
Losing weight without trying happens more often with IBD. During flares, your body struggles to absorb nutrients properly. You might also lose your appetite. With IBS, weight loss isn't typical unless you're avoiding many foods to manage your symptoms.
Feeling feverish and exhausted points toward IBD when inflammation is active. Your immune system is working overtime, leaving you drained in a way that rest can't fix. IBS can make you tired too, but it's different from the deep fatigue that comes with inflammation [3].
When your pain eases, it offers another clue. If your stomach feels better after a bowel movement, that suggests IBS. With IBD, the pain often lingers even after you go because of ongoing inflammation [9].
Waking up at night to rush to the bathroom is more common with IBD. Your symptoms don't follow a schedule when inflammation is involved. With IBS, your symptoms usually happen during the day, often after meals when your digestive system is active.
What lab tests show makes the distinction clear. Your practitioner looks for markers of inflammation in your blood and stool, like C-reactive protein (a general inflammation marker) and fecal calprotectin (which signals gut inflammation specifically). These levels rise with IBD but stay normal with IBS [8].
Your age when symptoms start may provide a hint. IBD often begins in your teens or twenties. IBS typically shows up in young adulthood [1].
These differences can help guide a diagnosis, but what's happening at the bacterial level reveals even more about how these conditions work.
IBS gut bacteria vs. IBD: How they compare
Both IBS and IBD involve bacterial shifts in your gut microbiome. Research shows each can involve changes in gut bacteria and immune activity. But the patterns differ dramatically, both in severity and in what's actually happening in the gut [10], [11]. The following distinctions can help practitioners provide more targeted care.
IBS: Mild changes without inflammation
IBS may alter the community of microbes in your gut, but these changes tend to be subtle, inconsistent, and not inflammation-related. This is why anti-inflammatory medications that help IBD don't improve IBS symptoms. Instead, shifts are caused by other triggers, like stress.
Some people with IBS have [10], [12], [13]:
- Subtle drops in certain beneficial bacteria, rather than a massive loss of overall bacterial diversity
- Gas and bloating from bacterial fermentation of food in the gut
- Changes tied to gut motility, how fast or slow the digestive system moves food through after you eat
IBD: Major microbiome disruption
In IBD, the microbiome is out of balance due to bacterial shifts, which often trigger visible tissue injury, sustained immune activation, and pronounced inflammation [2], [7], [14]. Beyond its inflammatory signature, microbial patterns are also more predictable in people with IBD, even during remission [9]-[11], [15].
Research shows people with Crohn's disease or ulcerative colitis often have [10],[15]:
- Lower bacterial diversity, fewer types of bacteria overall
- A drop in beneficial species like Faecalibacterium prausnitzii, which helps calm inflammation
- An increase in disruptive bacteria, including certain species from the Enterobacteriaceae family
- Signs of instability marked by altered growth patterns compared with those of healthy people
These bacterial changes are linked to immune activation, directly contributing to inflammation and how the disease progresses over time. Each condition benefits from a healthy, balanced microbiome.
When IBD feels like IBS (and why it gets confusing)
Even when IBD appears under control, many people still don't feel well. Research shows that up to one-third of people with IBD in remission continue having IBS-like symptoms. Stomach pain. Bloating. Loose or unpredictable stools [16]. Doctors sometimes call this cluster of symptoms IBS in IBD because these patients still have IBD, but their symptoms look more like IBS.
The tricky part is that symptoms can linger despite a normal colonoscopy or stool markers. For some people, ongoing gut sensitivity, microbiome changes, and functional issues are the driver, not active inflammation [3].
Researchers believe this may happen because of [3], [13], [16]:
- Persistent microbiome changes—bacteria may not fully bounce back even after the gut lining heals
- Increased intestinal permeability—the gut barrier stays leaky, allowing bacterial products to interact more closely with immune and nerve cells
- Heightened nerve sensitivity—gut nerves remain overly reactive following inflammation, amplifying pain and urgency
- Ongoing microbe-immune interactions and altered gut–brain signaling—these can persist even when classic inflammatory markers are absent in a stool test
Why knowing the difference matters for your health
Treatment depends on getting the right diagnosis. Anti-inflammatory drugs used for IBD don't help IBS. IBS-targeted approaches usually don't calm an IBD flare.
Here's the critical part: With IBD, inflammation can progress even when symptoms feel manageable. Complications like bleeding and strictures (areas where the intestine narrows and may affect how food and waste move through) can develop. Many people manage these effectively with early care. In some cases, additional treatment may be needed.
IBS may be highly disruptive to your life. But it doesn't cause physical damage to the gut.
Understanding these differences can help you make more informed decisions about your treatment options and long-term health. From medication choices to personalized diets to emerging microbiome-based approaches.
Support for your digestive health
Whether you have IBS, IBD, or ongoing digestive symptoms that haven't been diagnosed yet, understanding your gut bacteria can provide valuable insights.
For people with IBS, a Gut Health Test may help identify imbalances contributing to their symptoms. For those with IBD, you can work with your practitioner to measure stool chemistry markers, such as calprotectin, using our Pro Gut Health Test. It can also help reveal whether beneficial anti-inflammatory bacteria have recovered during remission. If you have ongoing symptoms but no clear diagnosis yet, testing can provide objective data to share with your practitioner.
FAQ
Can IBS turn into IBD?
No, IBS can't turn into IBD. They're completely separate conditions with different causes. IBS is a functional disorder characterized by gut sensitivity and by how your gut and brain communicate. IBD is an immune-mediated disease in which chronic inflammation damages the digestive tract. Having IBS doesn't put you at a higher risk for IBD. That said, if your IBS symptoms suddenly change or get worse, especially if you notice blood in your stool or unexpected weight loss, check in with your doctor to rule out other conditions.
Can IBS cause leaky gut?
You may hear IBS linked to “leaky gut.” While not a medical diagnosis, doctors call it increased intestinal permeability, meaning the gut barrier is less tight than it should be.
IBS doesn’t cause leaky gut in the same way IBD does, but mild permeability changes may be linked to gut sensitivity, pain, and bloating. Supporting the microbiome and calming the gut–brain connection may help strengthen the gut barrier [9], [13].
In IBD, increased intestinal permeability results from ongoing inflammation and damage to the gut lining.
What's the difference between IBD and IBS blood in stool?
Bloody diarrhea is common with IBD because inflammation can negatively impact and cause ulcers in the gut lining. This can range from small amounts of bright red blood to significant bleeding. IBS typically doesn't cause blood in stool. If you have IBS symptoms and notice blood, contact your practitioner.
What is irritable bowel syndrome acid reflux?
Irritable bowel syndrome and acid reflux often occur together. Many people with IBS also experience GERD (gastroesophageal reflux disease). Each involves altered gut-brain signaling and can share triggers, like stress and certain foods. If you have irritable bowel syndrome GERD, working with a gastroenterologist can help develop a treatment plan that addresses your specific needs.
What causes post-infectious irritable bowel syndrome?
Post-infectious irritable bowel syndrome develops after a gastrointestinal infection, like food poisoning or stomach flu. The initial infection triggers changes in gut bacteria, increases gut permeability, and leaves nerves hypersensitive even after it clears. This type of IBS accounts for about 10 percent of all IBS cases [17].
Does a 30-day IBS diet plan help with symptoms?
A 30-day IBS diet plan typically involves identifying and eliminating trigger foods, then gradually reintroducing them to see how you feel. Many people try a low-FODMAP diet for the short term. It may help reduce fermentable carbohydrates that can drive symptoms. A dietitian can help you personalize the approach based on individual triggers and nutritional needs. It’s always best to consult your practitioner before making any major changes to your diet.

Trust your gut.
References
[1] P. Oka, H. Parr, B. Barberio, C. J. Black, E. V. Savarino, and A. C. Ford, “Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta-analysis,” The Lancet Gastroenterology & Hepatology, vol. 5, no. 10, pp. 908–917, Oct. 2020, doi: 10.1016/S2468-1253(20)30217-X.
[2] R. R. Nathani, S. Sodhani, and E. Goosenberg, “Irritable Bowel Syndrome,” in StatPearls, Treasure Island (FL): StatPearls Publishing, 2025. Accessed: Feb. 06, 2026. [Online]. Available: http://www.ncbi.nlm.nih.gov/books/NBK534810/
[3] J. Wellens, J. Sabino, T. Vanuytsel, J. Tack, and S. Vermeire, “Recent advances in clinical practice: mastering the challenge—managing IBS symptoms in IBD,” Gut, vol. 74, no. 2, pp. 312–321, Feb. 2025, doi: 10.1136/gutjnl-2024-333565.
[4] Y. Fu, N. Waghray, R. Fass, and G. Song, “Diagnostic Implications of Irritable Bowel Syndrome Is an Independent Risk Factor for Undergoing Surgical Interventions in Patients with Inflammatory Bowel Disease,” Diagnostics, vol. 13, no. 11, May 2023, doi: 10.3390/diagnostics13111901.
[5] R. Wang, Z. Li, S. Liu, and D. Zhang, “Global, regional and national burden of inflammatory bowel disease in 204 countries and territories from 1990 to 2019: a systematic analysis based on the Global Burden of Disease Study 2019,” BMJ Open, vol. 13, no. 3, p. e065186, Mar. 2023, doi: 10.1136/bmjopen-2022-065186.
[6] E. Diez-Martin et al., “Inflammatory Bowel Disease: A Comprehensive Analysis of Molecular Bases, Predictive Biomarkers, Diagnostic Methods, and Therapeutic Options,” International Journal of Molecular Sciences, vol. 25, no. 13, Jun. 2024, doi: 10.3390/ijms25137062.
[7] C. McDowell, U. Farooq, and M. Haseeb, “Inflammatory Bowel Disease,” in StatPearls, Treasure Island (FL): StatPearls Publishing, 2025. Accessed: Feb. 06, 2026. [Online]. Available: http://www.ncbi.nlm.nih.gov/books/NBK470312/.
[8] L. Moraes et al., “Systemic Inflammatory Protein Profiles Distinguish Irritable Bowel Syndrome (IBS) and Ulcerative Colitis, Irrespective of Inflammation or IBS-Like Symptoms,” Inflamm Bowel Dis, vol. 26, no. 6, pp. 874–884, May 2020, doi: 10.1093/ibd/izz322.
[9] V. Stanisic and E. M. Quigley, “The overlap between IBS and IBD – what is it and what does it mean?,” Expert Review of Gastroenterology & Hepatology, vol. 8, no. 2, pp. 139–145, Feb. 2014, doi: 10.1586/17474124.2014.876361.
[10] A. Vich Vila et al., “Gut microbiota composition and functional changes in inflammatory bowel disease and irritable bowel syndrome,” Sci Transl Med, vol. 10, no. 472, p. eaap8914, Dec. 2018, doi: 10.1126/scitranslmed.aap8914.
[11] P. Szałwińska, J. Włodarczyk, A. Spinelli, J. Fichna, and M. Włodarczyk, “IBS-Symptoms in IBD Patients—Manifestation of Concomitant or Different Entities,” J Clin Med, vol. 10, no. 1, p. 31, Dec. 2020, doi: 10.3390/jcm10010031.
[12] X. Cheng, C. Ren, X. Mei, Y. Jiang, and Y. Zhou, “Gut microbiota and irritable bowel syndrome: status and prospect,” Front. Med., vol. 11, Oct. 2024, doi: 10.3389/fmed.2024.1429133.
[13] R. Spiller and G. Major, “IBS and IBD — separate entities or on a spectrum?,” Nat Rev Gastroenterol Hepatol, vol. 13, no. 10, pp. 613–621, Oct. 2016, doi: 10.1038/nrgastro.2016.141.
[14] E. Sinagra et al., “Inflammation in irritable bowel syndrome: Myth or new treatment target?,” World Journal of Gastroenterology, vol. 22, no. 7, pp. 2242–2255, Feb. 2016, doi: 10.3748/wjg.v22.i7.2242.
[15] S. Sultan, M. El-Mowafy, A. Elgaml, T. A. E. Ahmed, H. Hassan, and W. Mottawea, “Metabolic Influences of Gut Microbiota Dysbiosis on Inflammatory Bowel Disease,” Front. Physiol., vol. 12, Sep. 2021, doi: 10.3389/fphys.2021.715506.
[16] K. M. Fairbrass, S. J. Costantino, D. J. Gracie, and A. C. Ford, “Prevalence of irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease in remission: a systematic review and meta-analysis,” The Lancet Gastroenterology & Hepatology, vol. 5, no. 12, pp. 1053–1062, Dec. 2020, doi: 10.1016/S2468-1253(20)30300-9.
[17] G. Barbara et al., “Rome Foundation Working Team Report on Post-Infection Irritable Bowel Syndrome,” Gastroenterology, vol. 156, no. 1, pp. 46-58.e7, Jan. 2019, doi: 10.1053/j.gastro.2018.07.011.

