Having a baby is full of big moments, and we know that a C-section can come with its own set of challenges. That's why we're excited to share the results of our first clinical study, Infant Restore, which demonstrated that early gut health support may help reduce risks of microbiome-related diseases in babies born via C-section.
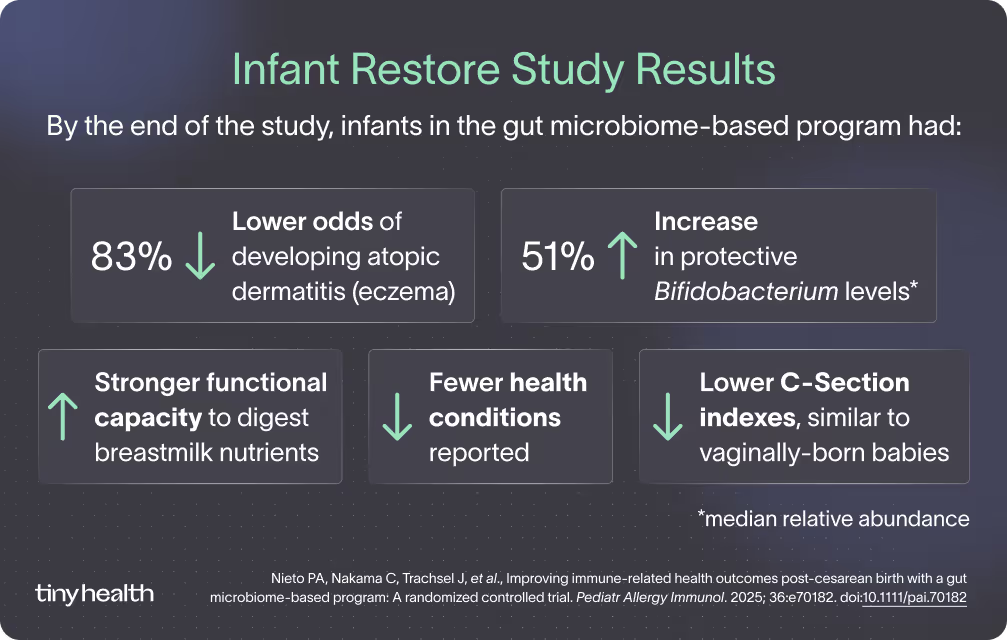
The research study, published in the medical journal Pediatric Allergy and Immunology, showed that participating in Tiny Health’s 6-month gut health support program reduced babies’ odds of developing atopic dermatitis (eczema) by 83% [1].
Just 6% of babies in the intervention group developed eczema, compared to 29% in the control group. Read on about how supporting your baby’s gut health early on may reduce their risk of immune-related conditions and give them a better foundation for lifelong health.
Infant Restore: what we studied
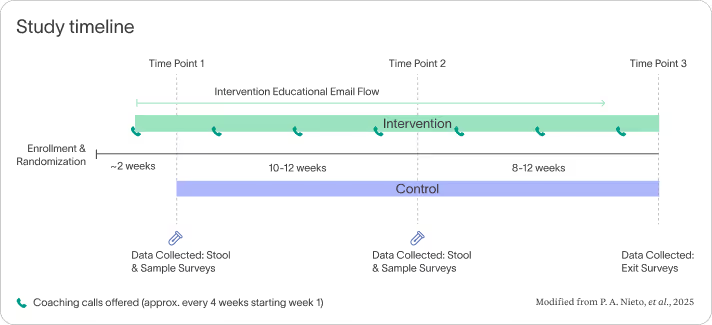
We followed 54 full-term infants for a period of six months. All the babies were delivered by C-section, and were under 3 months old when the study started. We randomly split the families into two groups. Twenty-five babies received personalized gut health support from Tiny Health, while 29 babies didn't participate in the program, allowing us to compare the results.

Parents in both groups took two Baby Gut Health Tests by collecting stool samples from their baby's diaper at the beginning of the study and again after three months. The program for the intervention group included a detailed analysis of their baby's gut bacteria, personalized advice on nutrition and probiotics, educational content, and one-on-one support from microbiome specialists. Researchers tracked changes in the babies' gut bacteria and surveyed parents about their babies' health.
All recommendations in the intervention group were optional and designed to empower parents in making informed decisions rather than a fixed course of action.
Why C-section babies face higher risks
About one in three U.S. babies is born by C-section every year [2]. Unlike vaginal birth, C-section birth means babies may miss out on beneficial bacteria normally passed from mother to baby during childbirth [3]. Instead, their gut microbiome is often colonized with hospital and skin bacteria that can be antibiotic-resistant and linked to gut inflammation later in life.
Research shows that these early differences in the gut microbiome — the community of bacteria and other tiny organisms living in the digestive system — can last for years, and are associated with higher risks of eczema, allergies, asthma, and even conditions such as obesity and type 1 diabetes [3]–[6].
Our data show that early microbiome support during the critical first 1,000 days can shift gut bacterial patterns away from those associated with eczema and allergies.
Key findings beyond eczema
Reducing the odds of developing eczema by 83% is significant. But babies who received the intervention also showed several positive changes by the end of the study [1]:
- Higher levels of beneficial bacteria: Bifidobacterium reached a median relative abundance of 82% (a 51% increase from the first sample) compared with 55% in the control group
- Better nutrient processing: More genes in their microbiome for digesting HMOs, which are beneficial complex sugars in breastmilk
- Gut bacteria more similar to vaginal birth: Lower "C-section index" scores, meaning their gut bacteria composition trended toward those of vaginally-born babies
What this means for parents
For the estimated 1.2 million C-section babies born in the U.S. each year, these findings suggest early gut health interventions may significantly reduce chronic disease risk.
More than 20 million children in the U.S. now live with a diagnosed allergic condition [7]. Eczema alone affects up to 1 in 6 infants. It is the first step in the atopic march, the progression of allergic diseases from eczema to food allergies, hay fever, and eventually asthma [8].
By addressing gut imbalances early, parents can potentially disrupt or reverse this progression.
The Cost of Allergic Conditions
If you have an immune-related condition or you're a parent of a child with one, you're not alone. According to the CDC, over 100 million Americans have eczema, food allergies, or hay fever, and 28 million have asthma [7],[9]–[11].
Atopic diseases can be costly for families. If your child has severe eczema, food allergies, and asthma, you could be looking at costs of $18,246 per year [12]–[14].
But it's not just the medical bills—these conditions affect your whole family's life. There are doctor visits, medications, emergency room trips, days off work when your child is sick, missed school days, and the stress that comes with watching your child struggle.
Across the entire country, the costs add up to staggering numbers. When adjusting for 2024 costs, the annual economic burden is estimated at:
- $6.7 billion for eczema [12]
- $37 billion for childhood food allergies [13]
- $122 billion for asthma [14]
Infants in the intervention group of Infant Restore had 83% lower odds of developing eczema. Consider what it could mean if proactive, targeted microbiome support in infancy were to become standard care? In a clinic serving 1,000 children a year, this could mean the difference between 337 children developing these conditions versus 77 children—a fivefold reduction.
Building a healthier future for babies
Beyond reducing the odds of developing atopic dermatitis, C-section-born infants in the program showed significant improvements in their gut bacteria makeup and function, and reported fewer health conditions.
This study is a milestone for Tiny Health and is deeply personal to our team. Our CEO, Cheryl Sew Hoy, founded the company after experiencing firsthand the challenges of raising a C-section baby who struggled with eczema and food sensitivities. She wanted to turn what research shows—that course-correcting the gut during the first 1,000 days can profoundly shape a child's lifelong health [15]—into a reality for families.
These early results are very promising. We're already working on larger studies to expand on these findings. With a better understanding of gut bacteria and practical advice, personalized preventive care is now possible for every family.



