Think of your gut barrier as a fortress with walls, moats, and guards. Discover how your microbes build, defend, and repair this living defense system, what happens when it breaks down, and which gut test metrics reveal your barrier's strengths and vulnerabilities. Plus, six habits to keep it resilient.
The Gut Barrier: A Living Fortress Microbes Build, Defend, and Repair
Summary
Every day, your gut does remarkable work breaking down food, producing compounds that fuel cells, and training your immune system to recognize friend from foe. Essential to all this activity is your gut barrier. This highly specialized lining acts as your body's gatekeeper, keeping harmful substances out while letting nutrients flow in.
Your gut microbiome plays a central role in your digestive health. And protecting that system is your gut barrier's job. But understanding what it actually does isn't easy. So we’re bringing it to life with a metaphor.
Think of your gut barrier as a castle: the sturdy walls keep threats out, the moat provides extra protection, and the guards control what enters. But, like any fortress, it's not impenetrable. Sometimes, invaders breach the walls.
In this article, we're exploring:
- How your microbes build, defend, and repair your gut lining;
- Why maintaining this system matters much more than you think; and
- Evidence-backed habits that support this living fortress for whole-body health.
The lay of the land: small intestine vs. large intestine
Before we explore the castle itself, it helps to understand the landscape. Your gut is a single continuous tube, but each region has a distinct structure and function [1].
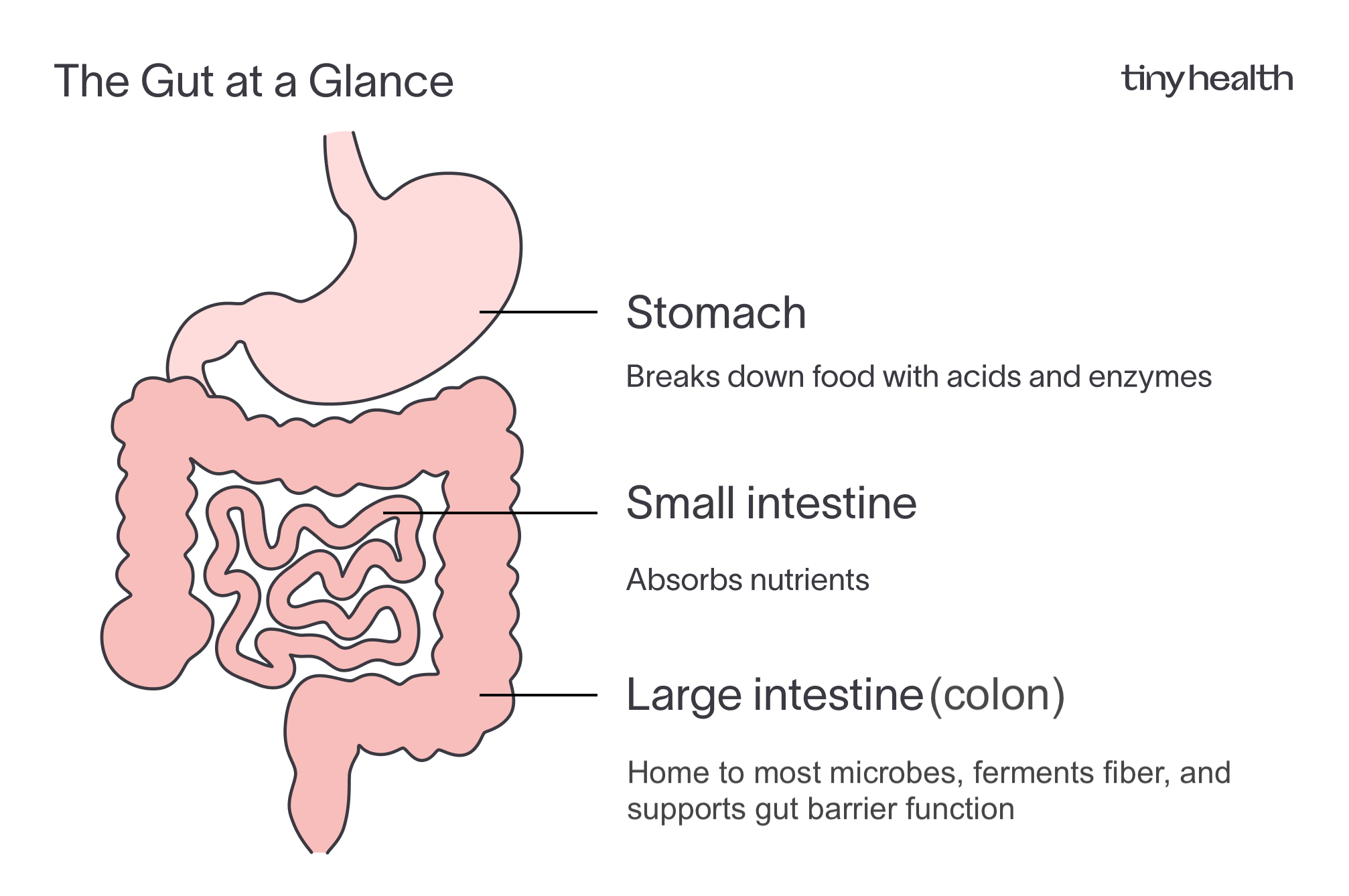
Small intestine
This is where most nutrient absorption happens. To do that efficiently, it’s built with:
- A thin, single mucus layer
- Looser connections between cells that allow nutrients, water, and electrolytes to pass
- Fewer microbes, since its main job is absorption, not fermentation
Large intestine (colon)
By the time food reaches the colon, most nutrients are gone, leaving fibers, water, and electrolytes. Here, the focus shifts from digestion to fermentation and protection. The colon has:
- A double mucus layer: an inner sterile layer pressed against the lining, and an outer layer where microbes thrive
- Tighter cell junctions that create a stronger barrier against unwanted visitors
- A dense, diverse microbiome that produces protective compounds like short-chain fatty acids (SCFAs)
Most gut microbes live in your colon, which is why a stool sample tells us so much about them. Think of the colon as the bustling city within the castle walls, home to your densest and most stable microbial communities. Bacteria ferment fiber, produce beneficial compounds, and help maintain a strong gut barrier. An at-home stool test lets us detect patterns that reveal whether your gut is balanced or disrupted, and how well your barrier is holding up.
The inner workings of your fortress
Every strong fortress depends on solid defenses, coordinated guards, and clear communication—key elements for your gut barrier, too. The castle’s walls, moat, and guards all work in harmony to protect and repair the kingdom. Your microbes are constantly talking, helping this living fortress stay strong. Here's how the metaphor breaks down.

Let's look a little closer at each layer.
Outer moat: The outer mucus layer is like the moat circling the castle. It’s filled with microbes, most living peacefully at the edge, keeping the castle safe by crowding out intruders.
Inner moat wall: Beneath the outer moat is a sterile inner mucus layer, a protective wall made of water and mucus molecules that keeps bacteria from reaching the lining.
Castle walls: These are the epithelial cells, the bricks of your gut barrier. Each one is sealed tightly to the next, forming a living barrier that’s both strong and selective. They let nutrients pass through the gates while keeping harmful intruders out.
Gate bolts: The tight junctions between these cells act like bolts holding the wall together. They’re not static; signals from beneficial microbes and their metabolites can tighten the junctions, while inflammation or excess toxins can loosen them.
Guardians: Friendly bacteria act as good citizens and peacekeepers. They train your immune system, keep harmful microbes in check, and help maintain balance.
Invading armies: Pathogenic bacteria and their harmful byproducts, such as hexa-LPS or excess hydrogen sulfide, are like enemy forces that can breach the walls if defenses weaken.
Wall masons: SCFA–producing bacteria, especially butyrate producers, are the workers who patch the walls, calm the guards, and provide fuel for the castle’s cells.
Supply lines: Dietary fibers and nutrients are the incoming supplies. Without them, the workers starve, repairs stall, and even the moat can shrink.
Some bacteria, like Bacteroides, are expert builders who help maintain the castle’s structure. But when they multiply too quickly, they can stir up inflammation [2]. Others, like Lactobacillus, act as peacekeepers. They release calming signals that strengthen the walls and steady the guards [3], [4].
As you can see, it takes a lot of effort to keep this fortress running smoothly. Sometimes, though, defenses are neglected. Cracks begin to form. And invaders have the opportunity to press the walls and test the castle’s resilience. This brings us to what happens when things go wrong.
When the barrier breaks
.png)
Like any fortress, your gut's defenses can weaken if the walls aren't maintained. But there isn't just one way a fortress falls.
Sometimes the moat drains faster than it refills. Sometimes cracks form between the stones. Other times, the guards overreact and cause more damage than the intruders themselves. In each case, invaders gain the upper hand, and the immune system springs into battle. In the gut, these scenarios play out through distinct types of barrier breakdown.
Mucus degradation – the drying moat: If too many microbes feed on the mucus layer faster than it can be replenished, the moat thins and bacteria press closer to the castle walls.
Some residents, like Akkermansia, are skilled moat keepers. They gently trim the mucus to stimulate renewal. But when their numbers rise too high, or when your diet lacks fiber to rebuild the layer, the system tips from helpful upkeep to overuse, leaving the lining exposed and vulnerable [5].
Tight junction breakdown – the loosening bolts: The “bolts” holding the wall’s bricks together are tight junctions, proteins that seal the gaps between cells.
Inflammation, stress, and dietary additives can weaken these connections, allowing microbial fragments or food antigens to slip through [6]-[10]. Signals from beneficial microbes and their metabolites, like butyrate, normally help keep these bolts tightened. When that signaling falters, small cracks can spread into larger breaches.
Immune overreaction – the guards go to war: When the moat thins and cracks, bacteria and their byproducts reach the epithelial wall, triggering alarms from immune cells stationed behind it. These sentinels release cytokines, molecular warning flares that summon reinforcements but inflame the area [11].
If the alarm persists, the defense turns on itself. Continued immune activation weakens the barrier, fuels oxidative stress, and disrupts normal repair processes [12]. Over time, this cycle locks the gut in a loop of irritation and recovery. It essentially erodes the barrier’s stability.
Leaky gut: When inflammation persists, immune signals and microbial fragments enter circulation and reach distant organs, from skin to brain. These ripple effects underscore the critical role of your gut barrier in controlling inflammation and protecting your overall health.
“Leaky gut” typically refers to increased permeability in the small intestine, where junctions are naturally looser. In the colon, it's about barrier breakdown or mucosal inflammation. Erosion of the mucus layer or damage to tight junctions signals that the balance between residents and defenses is faltering.
When the gut lining weakens, even minor disturbances like a dairy-rich meal, a minor stomach bug, or a stressful day can trigger discomfort or inflammation. Keeping the moat deep and walls strong maintains calm inside the fortress and stability throughout the body.
Now that you understand how things go wrong, let's explore how to care for and maintain your gut barrier.
How strong is your castle? The gut barrier check-in
Even the most well-armed fortress needs inspection. Your gut barrier is no different. Our Gut Health Test pinpoints the microbes and pathways that strengthen—or compromise—your barrier's defenses.
These compounds leave clues to your gut’s overall condition. When analyzed together, they show whether your microbial community is building and repairing the walls. They also reveal if the microbes are keeping the guards calm or signaling strain.
In other words, they turn an invisible ecosystem into something we can detect and report. Here’s how:
Hexa-LPS (invader weapons): A form of bacterial lipopolysaccharide (LPS), Hexa-LPS acts like weaponry from enemy forces. When barrier defenses are strong, it stays contained. When levels rise or the lining weakens, these molecules can trigger inflammation and heighten immune system signals [13],[14].
Mucus degradation (moat erosion): The moat’s depth depends on how well mucus is renewed and maintained. Some bacteria naturally trim this layer to stimulate growth, but when their activity outpaces repair, the moat begins to thin. Tracking mucus-degrading activity helps reveal when this balance tips, an early sign that microbes are pressing too close to the lining and that the barrier may be losing its protective buffer [5].
Hydrogen Sulfide (H₂S)(chemical sabotage): Produced by certain bacteria, hydrogen sulfide can support normal signaling at low levels but becomes corrosive when overproduced [15]. Elevated levels point to chemical stress on the barrier and a shift toward an inflammatory state.
SCFAs (the repair crew): SCFAs, including butyrate, propionate, and acetate, reflect how well your gut’s repair system is functioning [16], [17]. Higher levels usually indicate an active, resilient microbiome, one that fuels the wall, calms the guards, and maintains balance inside the castle.
GABA (the messenger): Microbial GABA is a signaling molecule that helps the gut communicate with its own nervous and immune systems [18], [19]. Steady levels suggest smooth coordination within the castle; imbalance may point to disrupted communication between residents and guards.
Each of these signals tells part of the castle’s story: whether the moat is deep, the walls are secure, or the workers have the supplies they need.
By looking at these microbial markers, we can gauge how resilient your gut is. And offer evidence-based recommendations, like simple daily choices, that can fortify your gut barrier and restore balance.
6 habits for a thriving fortress
If you've received the results of your Gut Health Test, you now know your gut barrier’s strengths and weaknesses. Your personalized Action Plan is specific to your microbiome, and you have priority next steps to support your gut health. If you have signs of gut barrier stress, don’t panic. Your gut is resilient.
If you're waiting on results or haven't tested yet, we have you covered. Here are six habits that keep the friendly microbes in your castle happy, balanced, and focused on protecting your health.
- The repair crew runs on fiber: A steady supply of diverse fiber from vegetables, fruits, legumes, and whole grains fuel SCFA–producing bacteria that renew and tighten the barrier [20]-[23].
- Rebuild the moat: Prebiotic fibers like inulin and resistant starch, along with colorful, polyphenol-rich plants, help refill the mucus layer and support the microbes that live within it [21], [24],[25]. This combo protects the castle.
- Recruit peacekeepers: Fermented foods bring in new allies. Yogurt, kefir, kimchi, sauerkraut, and other cultured foods introduce beneficial microbes that help maintain order and reinforce immune balance [26]. Even small, consistent servings diversify your microbial community, train the guards to respond calmly, and keep the ecosystem at peace.
- Limit the attacks: Every fortress faces threats from the outside. Ultra-processed foods high in sugar, additives, and emulsifiers can erode the moat and feed the wrong microbes [9], [10]. Cutting back on these modern stressors preserves the wall’s integrity and gives the beneficial citizens space to thrive.
- Keep the castle active: Movement keeps supplies circulating, and defenses alert. Regular physical activity supports gut motility, strengthens circulation, and encourages a more diverse microbiome [27], [28]. Regular exercise helps your castle stay dynamic, resilient, and ready for whatever comes its way.
- Guard against external stressors: Stress, lack of sleep, medications, and environmental toxins can all strain the moat and walls, tipping the balance. While not all of these factors can be avoided, managing stress, getting consistent rest, and using antibiotics and pain relievers only when needed can help the castle maintain stability and recover faster from disruptions.
Think of these six habits as bricks that work together to fortify the castle. Had some kimchi today? That’s one brick. Slept 8 hours last night? Another brick. Do your best as consistently as you can and keep this in mind: it’s a living fortress. That means it’s adaptive. Perfection isn’t the goal. Resilience is. You want a gut that bounces back from life’s ups and downs.
And these foundational habits are a great start.
For personalized insights and gut health guidance, our Tiny+ Adult Membership offers two tests: a baseline to show where you are now, and a follow-up to track how your daily habits affect your gut health over time. You'll also get a one-on-one session with a microbiome specialist.

Trust your gut.
References
[1] B. A. H. Jensen et al., “Small intestine vs. colon ecology and physiology: Why it matters in probiotic administration,” Cell Reports Medicine, vol. 4, no. 9, p. 101190, Sept. 2023, doi: 10.1016/j.xcrm.2023.101190.
[2] H. Zafar and M. H. Saier Jr, “Gut Bacteroides species in health and disease,” Gut Microbes, vol. 13, no. 1, p. 1848158, Jan. 2021, doi: 10.1080/19490976.2020.1848158.
[3] R. Huang et al., “Lactobacillus and intestinal diseases: Mechanisms of action and clinical applications,” Microbiological Research, vol. 260, p. 127019, July 2022, doi: 10.1016/j.micres.2022.127019.
[4] E. Dempsey and S. C. Corr, “Lactobacillus spp. for Gastrointestinal Health: Current and Future Perspectives,” Front. Immunol., vol. 13, Apr. 2022, doi: 10.3389/fimmu.2022.840245.
[5] A. M. Tingler and M.A. Engevik, M. A. Breaking down barriers: is intestinal mucus degradation by Akkermansia muciniphila beneficial or harmful? Infection and Immunity, 93(9), e0050324. https://doi.org/10.1128/iai.00503-24
[6] M. F. Neurath, D. Artis, and C. Becker, “The intestinal barrier: a pivotal role in health, inflammation, and cancer,” The Lancet Gastroenterology & Hepatology, vol. 10, no. 6, pp. 573–592, June 2025, doi: 10.1016/S2468-1253(24)00390-X.
[7] J. M. Allen et al., “Psychological stress disrupts intestinal epithelial cell function and mucosal integrity through microbe and host-directed processes,” Gut Microbes, vol. 14, no. 1, p. 2035661, Dec. 2022, doi: 10.1080/19490976.2022.2035661.
[8] S.-J. Leigh et al., “The impact of acute and chronic stress on gastrointestinal physiology and function: a microbiota–gut–brain axis perspective,” The Journal of Physiology, vol. 601, no. 20, pp. 4491–4538, 2023, doi: 10.1113/JP281951.
[9] P. Li et al., “Impacts of food additives on gut microbiota and host health,” Food Research International, vol. 196, p. 114998, Nov. 2024, doi: 10.1016/j.foodres.2024.114998.
[10] K. Whelan, A. S. Bancil, J. O. Lindsay, and B. Chassaing, “Ultra-processed foods and food additives in gut health and disease,” Nat Rev Gastroenterol Hepatol, vol. 21, no. 6, pp. 406–427, June 2024, doi: 10.1038/s41575-024-00893-5.
[11] C. Andrews, M. H. McLean, and S. K. Durum, “Cytokine Tuning of Intestinal Epithelial Function,” Front. Immunol., vol. 9, June 2018, doi: 10.3389/fimmu.2018.01270.
[12] C. Zeyneloglu et al., “The epithelial barrier theory proposes a comprehensive explanation for the origins of allergic and other chronic noncommunicable diseases,” FEBS Letters, vol. 599, no. 22, pp. 3208–3243, 2025, doi: 10.1002/1873-3468.70113.
[13] S. Mohammad and C. Thiemermann, “Role of Metabolic Endotoxemia in Systemic Inflammation and Potential Interventions,” Front. Immunol., vol. 11, Jan. 2021, doi: 10.3389/fimmu.2020.594150.
[14] F. Di Lorenzo, C. De Castro, A. Silipo, and A. Molinaro, “Lipopolysaccharide structures of Gram-negative populations in the gut microbiota and effects on host interactions,” FEMS Microbiol Rev, vol. 43, no. 3, pp. 257–272, May 2019, doi: 10.1093/femsre/fuz002.
[15] A. G. Buret, T. Allain, J.-P Motta, and J.L. Wallace. (2022). “Effects of hydrogen sulfide on the microbiome: From toxicity to therapy.” Antioxidants & Redox Signaling, Vol. 36, No. 4-6, pp. 211–219, February, 2022, doi: 10.1089/ars.2021.0004
[16] K. E. Hays, J. M. Pfaffinger, and R. Ryznar, “The interplay between gut microbiota, short-chain fatty acids, and implications for host health and disease,” Gut Microbes, vol. 16, no. 1, p. 2393270, Dec. 2024, doi: 10.1080/19490976.2024.2393270.
[17] D. Zhang et al., “Short-chain fatty acids in diseases,” Cell Commun Signal, vol. 21, no. 1, p. 212, Aug. 2023, doi: 10.1186/s12964-023-01219-9.
[18] D. Belelli, J. J. Lambert, M. L. Y. Wan, A. R. Monteiro, D. J. Nutt, and J. D. Swinny, “From bugs to brain: unravelling the GABA signalling networks in the brain–gut–microbiome axis,” Brain, vol. 148, no. 5, pp. 1479–1506, May 2025, doi: 10.1093/brain/awae413.
[19] P. Strandwitz et al., “GABA-modulating bacteria of the human gut microbiota,” Nat Microbiol, vol. 4, no. 3, pp. 396–403, Mar. 2019, doi: 10.1038/s41564-018-0307-3.
[20] H. D. Holscher, “Dietary fiber and prebiotics and the gastrointestinal microbiota,” Gut Microbes, vol. 8, no. 2, pp. 172–184, Mar. 2017, doi: 10.1080/19490976.2017.1290756.
[21] K. Makki, E. C. Deehan, J. Walter, and F. Bäckhed, “The Impact of Dietary Fiber on Gut Microbiota in Host Health and Disease,” Cell Host & Microbe, vol. 23, no. 6, pp. 705–715, June 2018, doi: 10.1016/j.chom.2018.05.012.
[22] K. Hodgkinson et al., “Butyrate’s role in human health and the current progress towards its clinical application to treat gastrointestinal disease,” Clinical Nutrition, vol. 42, no. 2, pp. 61–75, Feb. 2023, doi: 10.1016/j.clnu.2022.10.024.
[23] J. K. Tan, L. Macia, and C. R. Mackay, “Dietary fiber and SCFAs in the regulation of mucosal immunity,” Journal of Allergy and Clinical Immunology, vol. 151, no. 2, pp. 361–370, Feb. 2023, doi: 10.1016/j.jaci.2022.11.007.
[24] Z.-W. Guan, E.-Z. Yu, Q. Feng, Z.-W. Guan, E.-Z. Yu, and Q. Feng, “Soluble Dietary Fiber, One of the Most Important Nutrients for the Gut Microbiota,” Molecules, vol. 26, no. 22, Nov. 2021, doi: 10.3390/molecules26226802.
[25] F. Meiners, A. Ortega-Matienzo, G. Fuellen, and I. Barrantes, “Gut microbiome-mediated health effects of fiber and polyphenol-rich dietary interventions,” Front. Nutr., vol. 12, Aug. 2025, doi: 10.3389/fnut.2025.1647740.
[26] V. Valentino et al., “Fermented foods, their microbiome and its potential in boosting human health,” Microbial Biotechnology, vol. 17, no. 2, p. e14428, 2024, doi: 10.1111/1751-7915.14428.
[27] V. Monda et al., “Exercise Modifies the Gut Microbiota with Positive Health Effects,” Oxidative Medicine and Cellular Longevity, vol. 2017, no. 1, p. 3831972, 2017, doi: 10.1155/2017/3831972.
[28] M. Clauss, P. Gérard, A. Mosca, and M. Leclerc, “Interplay Between Exercise and Gut Microbiome in the Context of Human Health and Performance,” Front. Nutr., vol. 8, June 2021, doi: 10.3389/fnut.2021.637010.

