There's no single "perfect" gut microbiome, healthy guts vary based on your unique history, diet, and lifestyle. However, specific patterns, such as low SCFA production, elevated inflammation markers, and poor resilience, clearly signal imbalance. Testing helps identify where your microbiome needs support and provides personalized guidance to restore balance and optimize your gut health.
What Is an Ideal Gut Microbiome? (And Does One Even Exist?)

Summary
One of the most common questions we hear from people in and beyond our community is “What’s considered an ideal microbiome?” It's an interesting question, but one that rarely comes up in other areas of health.
Think about it: Doctors don't pinpoint the perfect cholesterol level for every patient. And a universal blood pressure that works for everyone does not exist. Yet no one would argue that an LDL of 350 or a blood pressure of 180/110 is a normal variation.
The same principle applies to your gut microbiome. There are many nuances to what’s considered healthy. And none of them mean perfect or ideal.
Why isn't there one "perfect" microbiome?
Your gut microbiome is complex, individualized, and shaped by your unique history, diet, culture, lifestyle, and genetics. In that sense, it really is like a fingerprint. There are many different ways a healthy gut can look.
While there’s no single perfect microbiome, that doesn’t mean there are no patterns of imbalance or dysfunction.
How do I know if my gut needs help?
While healthy microbiomes can look different from person to person, certain patterns clearly signal when balance is off. Tiny Health’s Gut Health Test highlights many key areas so you can understand what your results mean and where your microbiome may need support. Here are some examples.
Lack of SCFA production
If a microbiome lacks the ability to produce short-chain fatty acids (SCFAs), that’s a red flag. SCFAs are key molecules produced by beneficial gut bacteria when they digest fiber [1]. They fuel gut cells, protect the gut lining, support brain health as well as your overall well-being. If your microbiome isn’t making enough SCFAs, it’s a signal that targeted support could help restore balance.
Gut inflammation
Tiny Health has three Gut Inflammation markers that, when elevated, can signal issues with your gut barrier and inflammation. For example:
Hexa-LPS Index measures how much LPS—an inflammatory molecule made by certain gut bacteria —your gut may be exposed to. High levels can signal an increased risk of inflammation, especially if the gut barrier is weakened [2], [3].
Mucus Degradation Index reveals if your protective mucus lining is at risk of being worn down, leaving your gut wall exposed [4].
Hydrogen Sulfide index means excess gas production, which can irritate your gut lining and drain cellular energy [5].
Low Resilience
A resilient gut microbiome can bounce back from life’s ups and downs—like illness, antibiotics, or dietary changes. But when key protective species such as Faecalibacterium, Bifidobacterium, and certain Bacteroides are low or missing, your gut may have a harder time adapting to change.
For ages 3 and up, our Gut Resilience Score shows whether your microbiome has the diversity, functionality, and core species it needs to stay stable and recover from stress.
If your report shows low resilience, it means your microbiome could benefit from targeted support, like rebuilding beneficial species and improving overall diversity by eating more fiber-rich foods or taking probiotics.
For babies and toddlers under age 3, we look instead at the Maturation Index, which tracks healthy microbiome development for their age. In this stage, low levels of Bifidobacterium is not ideal, since these bacteria are vital for early gut health.
What’s the most common gut type?
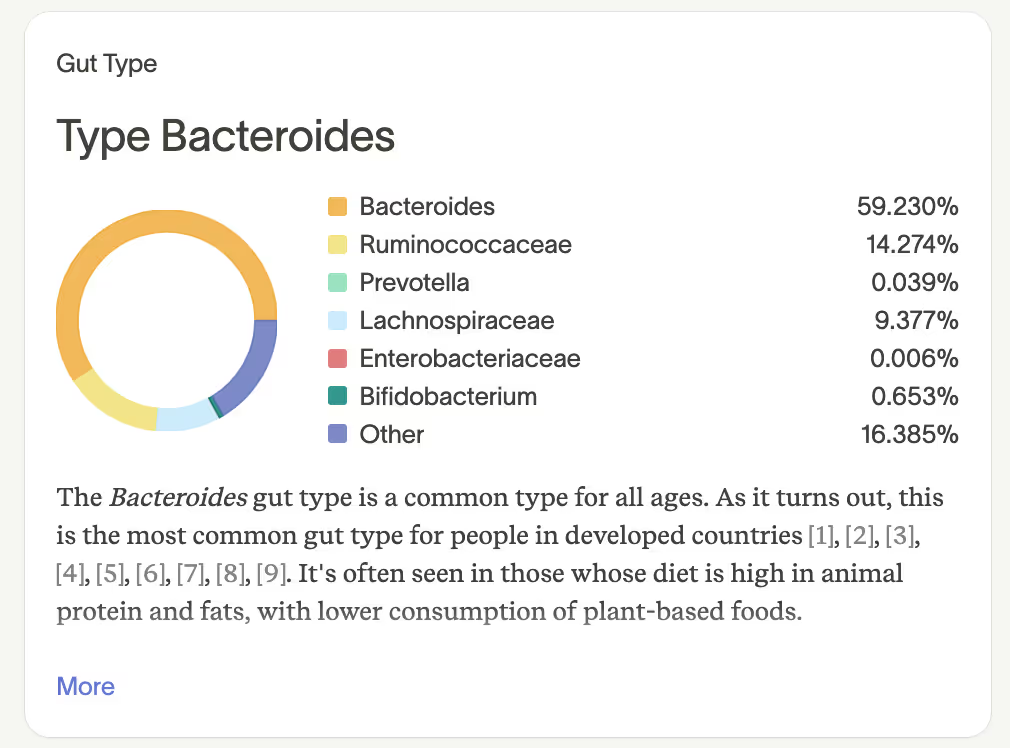
The Bacteroides gut type is one of the most common microbiome profiles, particularly in Western populations. It’s typical in diets high in animal protein and fats, with lower consumption of plant-based foods.
Is the Bacteroides gut type bad?
Not necessarily. A Bacteroides-dominant microbiome isn't inherently problematic—context matters. What's the overall diversity? Are beneficial bacteria present? Are you experiencing symptoms?
Can my gut microbiome change over time?
Yes! Your microbiome is dynamic and responds to changes in diet, stress, medications, and lifestyle. It can and often does bounce back. That means you have the power to influence your gut health.
So when should you test? If you have digestive issues, concerns about your gut health, or just want to optimize your diet based on your unique microbiome, testing can provide valuable insights. Getting your gut health baseline means having personalized insights to guide your health decisions and track your progress over time.
How often should I get a gut health test?
For adults, we recommend testing at least once a year. A lot can change in a few months— diet, stress levels, overseas travel, antibiotics, hormonal shifts, or new supplements can all impact your gut.
For children under 3, more frequent testing helps track the rapid changes happening in their developing microbiome. We recommend 3-4 tests during the first year if your budget allows, timed around key milestones like starting solids or after antibiotic treatments. This helps you understand how their gut is adapting and whether it needs extra support.
What do I actually do with my test results?
Every Tiny Health Gut Health Test includes a personalized, science-backed Action Plan with targeted guidance specific to your unique microbiome results. You'll receive practical recommendations across Diet, Lifestyle, and Supplement categories, all focused on what will make the greatest impact for your gut health.
Whether you're addressing a specific concern or optimizing overall wellness, these insights empower you to make confident, informed decisions about supporting your microbes. Plus, you can download a PDF to share with your practitioner.
What if my results aren’t good?
Your gut health is not static. If your test results show imbalances, your Action Plan will help you address them. In time, even small changes pay off. Plus, you can track your progress when you retest.
Remember, healthy does not mean perfect. Gut Health testing isn't about chasing an unattainable ideal. It's about using data from your test to guide more informed conversations with your practitioner and decisions about your gut health. Use it as a tool to understand your unique gut landscape, not as a diagnostic for disease.

Trust your gut.
References
[1] W. Fusco et al., “Short-Chain Fatty-Acid-Producing Bacteria: Key Components of the Human Gut Microbiota,” Nutrients, vol. 15, no. 9, p. 2211, May 2023, doi: 10.3390/nu15092211.
[2] S. H. Rhee, “Lipopolysaccharide: basic biochemistry, intracellular signaling, and physiological impacts in the gut,” Intest Res, vol. 12, no. 2, pp. 90–95, Apr. 2014, doi: 10.5217/ir.2014.12.2.90.
[3] S. S. Ghosh, J. Wang, P. J. Yannie, and S. Ghosh, “Intestinal Barrier Dysfunction, LPS Translocation, and Disease Development,” J Endocr Soc, vol. 4, no. 2, p. bvz039, Feb. 2020, doi: 10.1210/jendso/bvz039.
[4] M. S. Desai et al., “A Dietary Fiber-Deprived Gut Microbiota Degrades the Colonic Mucus Barrier and Enhances Pathogen Susceptibility,” Cell, vol. 167, no. 5, pp. 1339-1353.e21, Nov. 2016, doi: 10.1016/j.cell.2016.10.043.
[5] A. G. Buret, T. Allain, J.-P. Motta, and J. L. Wallace, “Effects of Hydrogen Sulfide on the Microbiome: From Toxicity to Therapy,” Antioxid Redox Signal, vol. 36, no. 4–6, pp. 211–219, Feb. 2022, doi: 10.1089/ars.2021.0004.

