Sarah, a homeschooling mom, struggled with her infant son Caleb’s eczema, colic, and sleep problems. After trying traditional care with no success, a Tiny Health gut microbiome test revealed bacterial imbalances. Following a personalized Action Plan that included probiotics, Caleb’s skin cleared, his sleep improved, and Sarah is now sharing her story to help other parents.
Case Study: How One Mom Found Answers to Eczema and Lost Sleep

Summary
Sarah is a former high school English teacher who now homeschools her three children. She describes her youngest, 22-month-old Caleb, as "ALL BOY" who is full of energy and always wants to be outside.
You wouldn't know it from this happy picture, but for over a year, Caleb had a series of symptoms that made his nighttime routine an exhausting time for the whole family. What started as colic at just two months old became ongoing sleep issues that lasted 14 months.
When doctors said, “He’ll grow out of it,” Sarah’s intuition told her otherwise. Around Caleb’s first birthday, he had a severe eczema outbreak, adding more worry to an already stressful situation.
After a frustrating year of conventional care and steroid treatments that only made things worse, Sarah shares how an Instagram post finally led to answers and relief for Caleb.
The start of nighttime crying spells
At two months, Caleb would cry inconsolably for hours every night. Nursing calmed him in the moment, but the next night, the screaming returned. “Sometimes he would squall for an hour. It was terrible. The pediatrician I had at the time kept telling me he would grow out of it, but since I have two older kids, I just felt that wasn’t true.”
Caleb never had issues during the day, so Sarah’s doctor didn’t think a gastroenterologist would help.
Yet, his symptoms persisted month after month. While his colic improved slightly at 6 months, Sarah hit a breaking point when Caleb was 10 months old. The stress and frustration over feeling alone in her search for answers couldn’t go on.
“I was at my wits' end with no sleep and took him to the ER of the closest children’s hospital.”
Sarah left with a referral to a GI specialist. “She was so nice, but after we ran the tests she recommended, everything came back fine, and she was at a loss as well.”
Sarah tried everything, from gas drops and belly massage to dairy elimination and propping him up while he slept. Nothing helped.
A severe eczema outbreak
Around Caleb’s first birthday, he broke out in a severe eczema rash. Sarah said he had a few small spots at 3 months old that had cleared up with lotion, but this was different. Each week, the rashes spread until he was covered from head to toe.
Sarah went to two dermatologists, but nothing improved. “The steroid treatment only caused it to come back worse after a few weeks, and his legs turned grayish/purple.”
Despite her mounting stress levels and exhaustion, Sarah kept looking for ways to soothe Caleb’s distress. But the eczema lotions, creams, and bathing routines offered no relief.
"Being a stay-at-home mom helped as far as not having work stress. But the emotional toll was truly awful. I cried every few days because of lack of sleep... it caused me to lash out more because I just had no patience."
Eventually, Sarah’s persistence paid off.
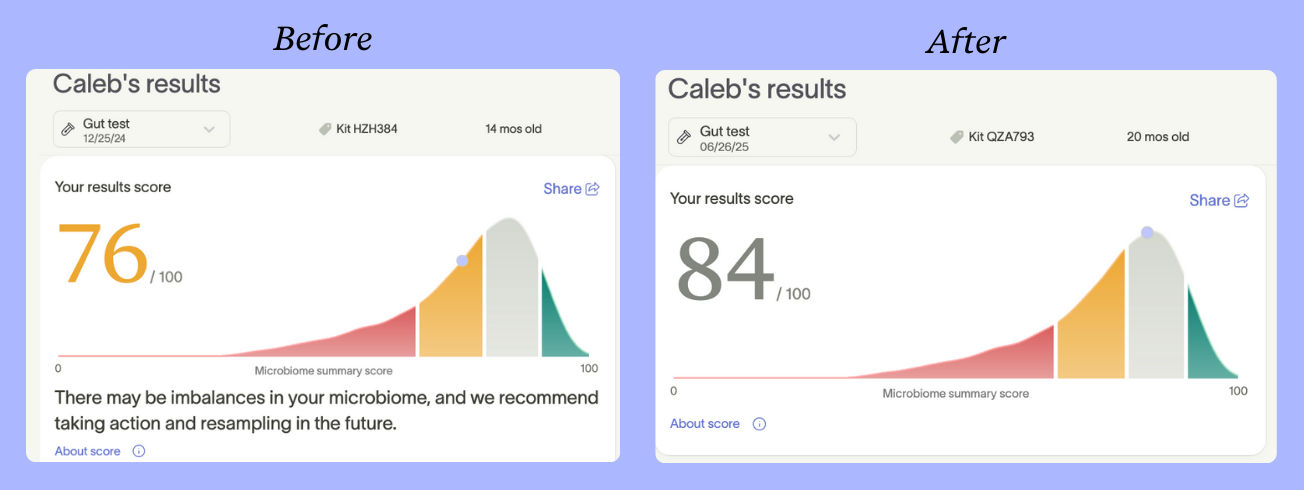
“A Tiny Health post came across my Instagram. I had read that eczema can be a gut problem, so I ordered the kit. I mailed it off the day after Christmas in 2024. He was 14 months old at the time and still waking up crying and screaming every 3-4 hours.”
What Caleb’s gut health tests revealed: before and after
On the results landing page of the customer portal, the first thing Sarah noticed was a high abundance of disruptive microbes. Sarah was alarmed. "He had an overgrowth of bad bacteria that was 2.5x higher than the normal range."
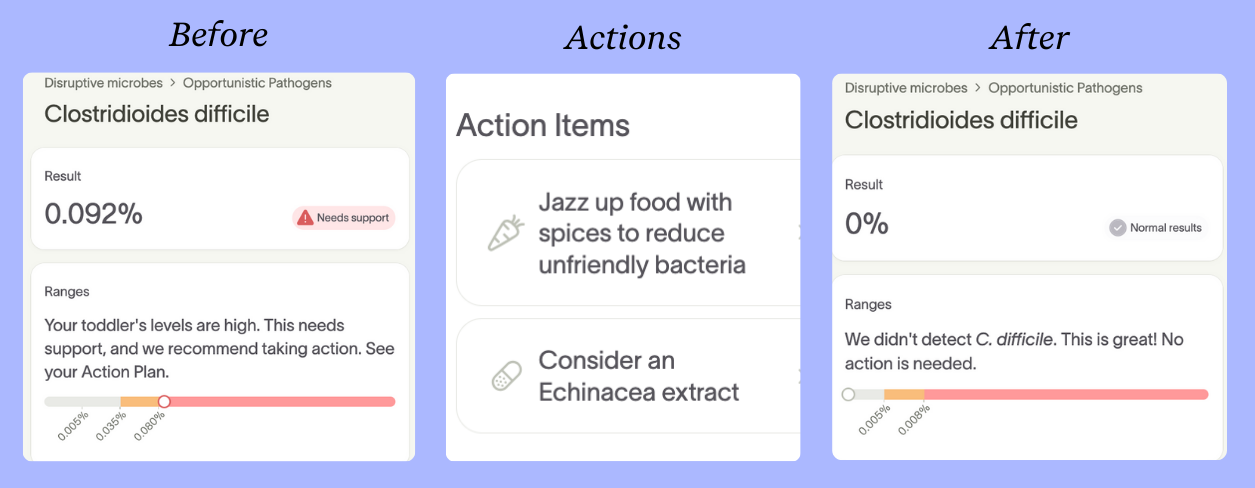
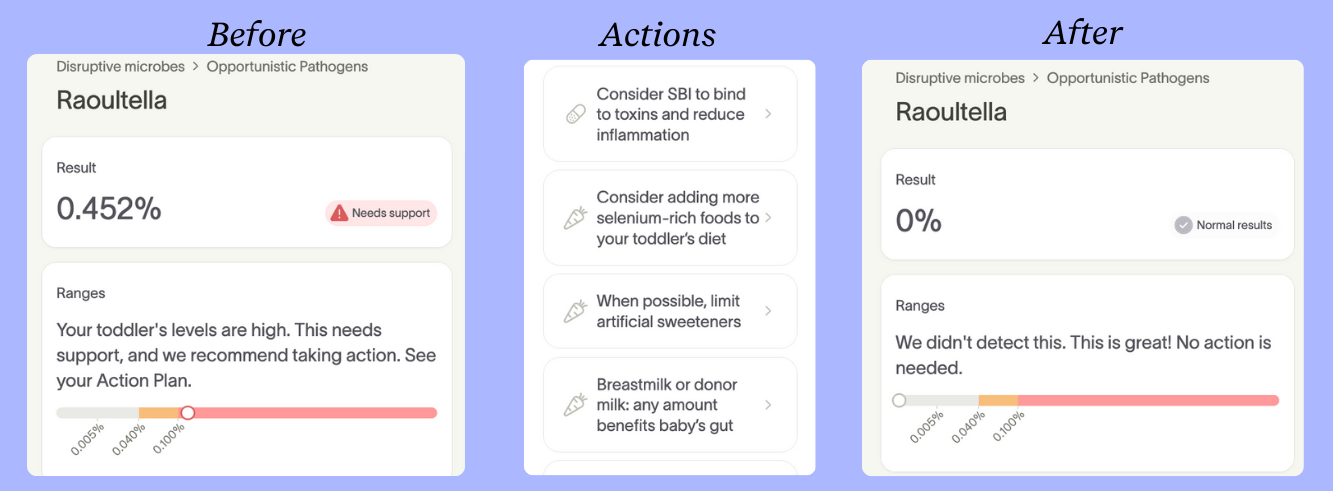
Caleb had two opportunistic pathogens that were flagged as needing support, Clostridioides difficile (also known as C. diff) and Raoultella. Sarah worked with microbiome specialist Lisa Hughes to discuss these results and next steps from Caleb’s Action Plan. They discussed how his birth history, which included a C-section and antibiotics, may lead to gut imbalances and the increased odds of microbiome-related conditions such as eczema [3].
While C. diff can normally reside in the gut at very low levels without causing problems, the elevated level from Caleb’s first test suggested an imbalance that required attention. C. diff is particularly concerning after antibiotic use, when it can multiply and cause severe diarrhea and digestive inflammation [1].
Sarah added the probiotic to his oatmeal each day for six weeks, supplementing it with breastmilk from her sister.
Caleb’s results also showed high levels of Raoultella. While its clinical role is still being studied, elevated levels have been reported in gut-related infections, which may contribute to symptoms like digestive discomfort, fussiness, or impaired nutrient absorption, especially in children with microbiome imbalances [2].
"It was such a relief! It made me feel like finally I had some kind of actual direction to go instead of feeling like I was walking through the dark trying to figure it out myself."
The improvements came sooner than Sarah expected: "Within two weeks, he was only waking up crying like once a night. It honestly felt like a miracle. Then, after two months from the time I started the protocol, his skin was completely clear."
Despite having imbalances, Caleb’s better-than-average first Microbiome Summary Score was a positive sign. With no evidence of C. diff or Raoultella bacteria in Caleb’s follow-up test, his score jumped 8 points.
The changes Sarah made to Caleb’s routine showed how resilient his gut is when given the right support.
From surviving to thriving
Looking back, Sarah reflects on how the extended period of sleep deprivation affected her. “I felt like a zombie for over a year and began to despair that it would never get better. I have basically no memories from that time of life because of my lack of sleep."
Today, Sarah is feeling much happier and more patient. And just as important, her memory is back.
While she’s thankful for the quality of life her family is now enjoying, Sarah did share some frustration over feeling isolated while searching for answers through traditional means.
"I felt like I had to navigate this journey mainly by myself, and that was really hard because I'm not a trained professional,” said Sarah. “I’m just a mom who loves her children.”
The more time passes, the more Sarah thinks about other families, “How many other children are unnecessarily suffering or taking the wrong treatments?"
As for Caleb’s future, Sarah is optimistic about managing his eczema and hopes that sharing his story gives other parents some much-needed hope.
Setting the foundation for lifelong health
If your little one is just starting out, supporting their gut microbiome early on may help protect against eczema and set the foundation for long-term health. Tiny Health's clinical trial, Infant Restore, found that a 6-month intervention program reduced the odds of eczema in C-section babies by 83%. Download our Infant Restore White Paper to learn more.
References
[1] CDC, “About C. diff,” C. diff (Clostridioides difficile), 18-Aug-2025. [Online]. Available: https://www.cdc.gov/c-diff/about/index.html. [Accessed: 07-Oct-2025].
[2] T. M. Appel, N. Quijano-Martínez, E. De La Cadena, M. F. Mojica, and M. V. Villegas, “Microbiological and Clinical Aspects of Raoultella spp.,” Front. Public Health, vol. 9, Aug. 2021, doi: 10.3389/fpubh.2021.686789.
[3] P. A. Nieto et al., “Improving immune-related health outcomes post-cesarean birth with a gut microbiome-based program: A randomized controlled trial,” Pediatric Allergy and Immunology, vol. 36, no. 9, p. e70182, 2025, doi: 10.1111/pai.70182.

